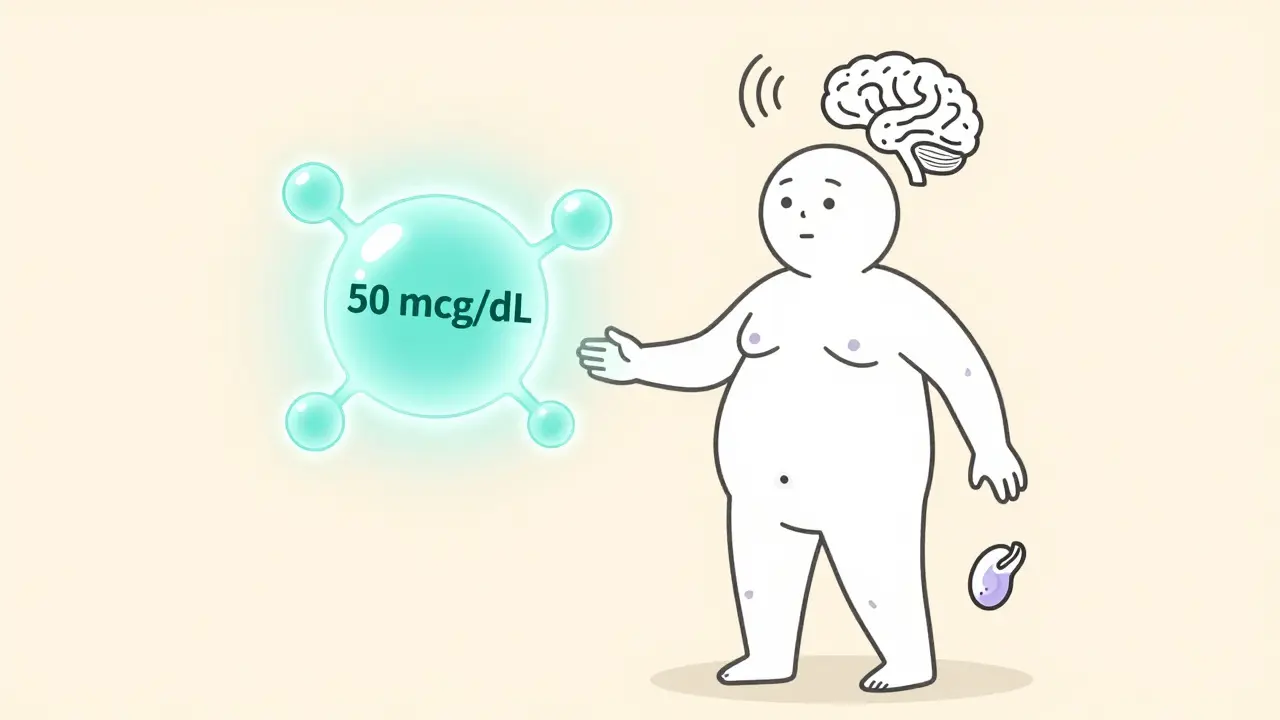
Cushing's syndrome isn't just weight gain or a round face. It’s a serious endocrine disorder caused by too much cortisol floating through your body for months or years. This hormone, made by your adrenal glands, normally helps you handle stress, control blood sugar, and manage inflammation. But when it’s too high-often above 50 mcg/dL in a 24-hour urine test, when the normal range is just 5-25 mcg/dL-it starts breaking down muscle, weakening bones, raising blood pressure, and turning your body inside out. The good news? If it’s caused by a tumor, surgery can fix it. The better news? When done right, it can bring your life back.
What Causes Cushing's Syndrome?
Most people with Cushing’s don’t realize they have it until symptoms pile up. You might notice your face getting rounder, your neck developing a fatty hump, or purple stretch marks appearing on your abdomen-even if you haven’t gained much weight overall. Your arms and legs stay thin while your torso swells. Blood pressure climbs. Blood sugar spikes. You get bruised easily. Women may stop having periods. Men lose libido. Osteoporosis creeps in without warning. These aren’t random side effects-they’re direct results of cortisol running wild. There are two main types. About 80% of cases come from taking steroid medications like prednisone for asthma, arthritis, or autoimmune diseases. That’s called exogenous Cushing’s, and it’s manageable by slowly reducing the dose. But the other 20%? That’s endogenous-your own body making too much cortisol. And that’s where surgery becomes the only real cure. Endogenous Cushing’s usually comes from one of three places:- Pituitary adenomas (60-70% of cases): A benign tumor in the pituitary gland overproduces ACTH, which tells the adrenal glands to make more cortisol. This is called Cushing’s disease.
- Adrenal tumors (15-20%): A tumor on one adrenal gland makes cortisol directly, without needing ACTH.
- Ectopic ACTH tumors (5-10%): Rare tumors in the lungs, pancreas, or thymus pump out ACTH like a broken faucet.
How Do Doctors Diagnose It?
Diagnosing Cushing’s isn’t quick. You need at least two positive tests because cortisol levels naturally rise and fall. The gold standard tests include:- Late-night salivary cortisol: Levels above 0.14 mcg/dL suggest abnormal production.
- 24-hour urine free cortisol: Over 50 mcg/24h is a red flag.
- Low-dose dexamethasone suppression test: If your cortisol stays above 1.8 mcg/dL after taking a steroid pill, your body isn’t responding like it should.
Why Surgery Is the First-Line Treatment
For endogenous Cushing’s, medication alone rarely fixes the root problem. Drugs like pasireotide or mifepristone can lower cortisol, but they’re expensive-$5,000 to $10,000 a year-and don’t shrink tumors. They’re a bridge, not a cure. Surgery is the only way to remove the source. The Endocrine Society, the American Association of Neurological Surgeons, and top hospitals like Mayo Clinic and OHSU all agree: if a tumor is found, surgery should come first. For pituitary tumors (Cushing’s disease), the procedure is transsphenoidal surgery. A surgeon goes through the nose or upper lip to reach the pituitary. No scalp incision. No brain opening. The surgery takes 2-4 hours. Hospital stay? Usually 2-5 days. Success rates depend on tumor size and surgeon experience. For microadenomas under 10 mm, remission happens in 80-90% of cases. For larger macroadenomas, it drops to 50-60%. The difference? Volume. Centers that do more than 20 pituitary surgeries a year have remission rates above 80%. Those doing fewer than 10? Only 50-60%. That’s not a small gap-it’s life-changing. For adrenal tumors, laparoscopic adrenalectomy is the go-to. A few small cuts, a camera, and the bad gland is removed. Recovery is faster-often just 1-2 days in the hospital. Success? About 95%. Complications? Less than 5%.What Happens After Surgery?
You might think removing the tumor means you’re done. Not even close. Your body has been flooded with cortisol for so long that your adrenal glands have shut down. After surgery, you go into temporary adrenal insufficiency. You’ll need hydrocortisone replacement for weeks or months. Some people need it for life. This isn’t just about taking pills. You need to learn how to adjust your dose during stress-illness, injury, even dental work. Missing a dose can lead to an adrenal crisis: vomiting, low blood pressure, passing out. It’s dangerous. That’s why 85% of patients at high-volume centers work with a dedicated Cushing’s nurse coordinator. At regular clinics? Only 65% follow the plan. Recovery takes time. Most people feel better in 3-6 months. Fatigue fades. Skin clears. Blood pressure drops. Weight comes off. But it’s not instant. Some patients report lingering issues-brain fog, joint pain, depression. A few need lifelong hormone replacement for thyroid, testosterone, or estrogen after bilateral adrenalectomy.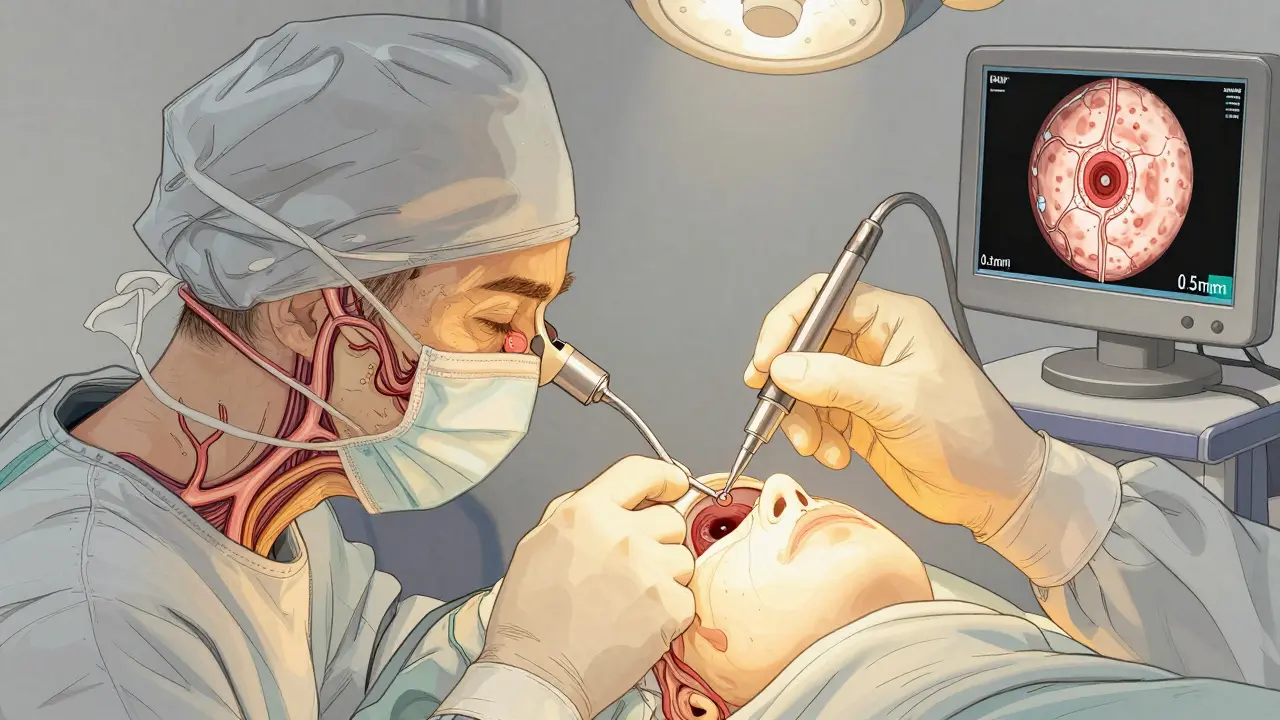
What Are the Risks?
Surgery isn’t risk-free. For transsphenoidal surgery:- CSF leak: Cerebrospinal fluid leaks out through the nose in 2-5% of cases. May need another surgery to fix.
- Adrenal insufficiency: Nearly all patients need steroids after. Permanent in 5-10%.
- Infection: Less than 3%.
- Recurrence: 10-25% of patients see cortisol levels rise again within 10 years.
- 100% cure-but you’ll need lifelong steroids.
- Nelson’s syndrome: A dangerous pituitary tumor grows in 40% of cases within 5 years.
Real People, Real Outcomes
On patient forums like the Cushing’s Support & Research Foundation, 687 people shared their stories. Of those who had pituitary surgery, 72% saw dramatic improvements within 3-6 months. One woman, Jane_D, wrote: “Two months after surgery, my moon face vanished. My blood pressure dropped to normal without meds. I lost 40 pounds.” But 28% struggled. Mark_T, 38, said: “I still have chronic fatigue. I need thyroid and testosterone replacements now.” A 2022 Reddit survey of 312 surgical patients showed 65% would do it again. Why? Because they avoided heart attacks, broken bones, or strokes that were coming. One man’s bone density improved from T-score -3.5 (severe osteoporosis) to -1.8 (normal) in a year.Who Should Get Surgery? And When?
If you have endogenous Cushing’s and a tumor, surgery is your best shot. But timing matters. Dr. Edward Laws, a leading pituitary surgeon, found that patients who get surgery within two years of diagnosis have 30% higher remission rates than those who wait. Don’t wait for symptoms to get worse. High cortisol kills. Even after successful surgery, your mortality risk stays 1.5-2 times higher than the general population. That’s why follow-up care is non-negotiable. You need to be treated at a center that does at least 20 pituitary surgeries a year. Ask: “How many Cushing’s cases do you handle annually?” If they don’t know, find someone who does.
What’s New in Cushing’s Surgery?
Technology is improving outcomes. In 2023, the FDA approved a new 3D endoscopic system called the Neuro-Robotic Scope. It gives surgeons 0.5mm resolution and cuts CSF leak rates by 40%. Another tool, 11C-metomidate PET/CT, is in trials and can find tumors with 95% accuracy-up from 70% with old scans. The NIH’s CUREnet registry is tracking over 1,000 patients. Early data shows if you get surgery within 18 months of diagnosis, your chance of remission is 85%. Wait past 24 months? It drops to 65%.What If Surgery Doesn’t Work?
About 20-30% of patients need a second surgery. Others turn to radiation, like stereotactic radiosurgery, or medications. Some end up with bilateral adrenalectomy as a last resort. It’s not ideal-but it saves lives. The goal isn’t just to lower cortisol. It’s to restore your life. To walk without pain. To sleep through the night. To stop being afraid of your own body.Final Thoughts
Cushing’s syndrome isn’t just a medical condition. It’s a thief. It steals your strength, your confidence, your health. But it can be stopped. Surgery, when done early and by the right team, is the most powerful tool we have. It doesn’t guarantee perfection-but it gives you back your future.Can Cushing’s syndrome be cured without surgery?
If Cushing’s is caused by steroid medications (exogenous), then yes-gradually reducing or stopping the drugs can reverse it. But if it’s caused by a tumor inside your body (endogenous), medication alone rarely cures it. Drugs like pasireotide or mifepristone can lower cortisol levels, but they don’t remove the tumor, often have side effects, and cost $5,000-$10,000 a year. Surgery is the only treatment that targets the root cause and offers a real chance at long-term remission.
How long does recovery take after Cushing’s surgery?
Most people start feeling better within 3-6 months, but full recovery can take up to a year. Fatigue, mood swings, and muscle weakness fade slowly as your body readjusts to normal cortisol levels. You’ll need steroid replacement for weeks or months, and your dose must be carefully adjusted. Returning to work often takes 4-8 weeks for pituitary surgery and 2-4 weeks for adrenal surgery, but full energy levels may take longer. Patience and follow-up care are critical.
What are the chances of Cushing’s coming back after surgery?
Recurrence rates vary by tumor type and surgical center. For pituitary microadenomas treated at high-volume centers, recurrence is about 10-15% over 10 years. For macroadenomas, it’s higher-up to 25%. Adrenal tumors have a lower recurrence rate, around 5-10%, because the source is removed. If cortisol levels rise again, you may need a second surgery, radiation, or lifelong medication. Regular follow-up blood and urine tests are essential for early detection.
Why does surgeon experience matter so much in Cushing’s surgery?
Pituitary tumors are tiny-sometimes smaller than a pea-and sit deep in the skull. Finding and removing them without damaging nearby nerves, blood vessels, or the normal pituitary gland requires extreme precision. Surgeons at high-volume centers (doing 20+ cases a year) have refined their techniques over hundreds of procedures. Studies show their remission rates are 80-90%, while low-volume centers average only 50-60%. That difference isn’t just numbers-it’s whether you get your life back or face repeat surgeries and complications.
Is bilateral adrenalectomy a good option?
Bilateral adrenalectomy removes both adrenal glands and cures Cushing’s in 100% of cases. But it’s a last-resort option because it means you’ll need lifelong hormone replacement for cortisol and aldosterone. There’s also a 40% risk of developing Nelson’s syndrome-a fast-growing pituitary tumor that can cause vision loss and severe headaches. This procedure is usually reserved for patients who’ve failed other treatments or have aggressive, widespread disease. It saves lives, but it changes them permanently.
What should I look for in a surgical center for Cushing’s?
Ask three things: How many Cushing’s surgeries do you perform each year? Do you have a dedicated endocrine surgical team? Do you offer post-op coordination with endocrinologists and nurses? The Endocrine Society recommends centers doing at least 20 pituitary surgeries annually. High-volume centers have better outcomes, fewer complications, and better support systems. Avoid centers that treat Cushing’s as an afterthought-it’s a complex condition that needs specialists.
Can Cushing’s syndrome cause permanent damage even after surgery?
Yes. Long-term high cortisol can cause irreversible damage to bones, blood vessels, and organs. Even after successful surgery, some patients are left with osteoporosis, high blood pressure, or type 2 diabetes that require ongoing treatment. That’s why early diagnosis and treatment are so important-the sooner you act, the less damage accumulates. Regular follow-up with bone density scans, heart checks, and blood sugar monitoring is essential for long-term health.




8 Comments
This post literally made me cry. I had Cushing’s for 5 years and no one believed me until my cortisol hit 78. Surgery saved my life-now I can sleep through the night without feeling like my bones are dissolving. Thank you for writing this.
Look, I’ve read every paper on ACTH-dependent vs. non-dependent Cushing’s since 2018, and let me tell you-most clinicians don’t even understand the hypothalamic-pituitary-adrenal axis dynamics. You’re talking about a neuroendocrine cascade that’s been dysregulated for years, and yet people think it’s just ‘weight gain’? No. It’s molecular chaos. The adrenal cortex becomes hypersensitive to ACTH, the glucocorticoid receptor signaling gets downregulated, and your liver starts gluconeogenesis on overdrive. And don’t even get me started on the epigenetic modifications from chronic hypercortisolism. Surgery isn’t just ‘fixing a tumor’-it’s resetting an entire hormonal identity. Most patients don’t realize they’re not just losing fat-they’re reclaiming their autonomic nervous system. The fact that 85% of high-volume centers have nurse coordinators? That’s not ‘support,’ that’s trauma-informed endocrine care. And if you’re not getting dexamethasone-CRH testing before surgery, you’re basically flying blind. This isn’t medicine-it’s precision warfare against your own body.
Everyone’s so excited about surgery like it’s a magic wand-what about the people who get it and still feel like garbage? I had transsphenoidal surgery in 2021. My cortisol’s normal. My face is back. But I’m still on 30mg hydrocortisone, my libido’s dead, and I can’t lift my own damn groceries. You don’t talk about the ghost limb syndrome of cortisol. It’s not gone-it’s haunting you.
Just wanted to add a clinical note: the 2023 meta-analysis in JCEM showed that preoperative ACTH levels >100 pg/mL predict higher recurrence risk post-transsphenoidal surgery, regardless of tumor size. Also, 11C-metomidate PET/CT has a 92% sensitivity for adrenal adenomas-way better than CT/MRI. If your center doesn’t offer it, push for it. And yes, bilateral adrenalectomy isn’t ‘last resort’-it’s the only option when you’ve had 3 failed surgeries and Nelson’s is looming. Don’t romanticize surgery; optimize it.
So surgery fixes it? Cool. What’s the cost? And how many people die from the surgery itself? You guys act like it’s a nose job.
Thank you for this. 🙏 I’m a nurse in an endocrine clinic and I see this every day. The biggest thing patients need isn’t just surgery-it’s someone who listens. After surgery, they’re terrified to adjust their steroid dose because they’ve been told ‘one wrong pill and you die.’ We need more coordinated care teams. Also, if you’re reading this and you’re scared-your feelings are valid. But you’re not alone. There’s a whole community out here cheering you on. You got this.
So let me get this straight-you’re telling me the best way to cure a disease caused by too much cortisol… is to surgically remove the source and then give the patient cortisol for the rest of their life? That’s not a cure. That’s a very expensive, very invasive game of whack-a-mole with your own adrenal glands. Maybe we should just all take a nap and let nature fix it? 🤔
Recurrence rates 10-25%? That’s not good. Why not just remove the adrenals first? Less hassle.