Chronic muscle pain that won’t go away? You might not have a pinched nerve or a herniated disc. You could be dealing with myofascial pain syndrome - a condition hiding in plain sight, often mistaken for something else. It’s not just soreness. It’s deep, aching, and radiates in strange patterns - like pain shooting from your shoulder into your hand, or headaches that start at the base of your skull. This isn’t random. It’s triggered by tight knots in your muscles called trigger points.
What Exactly Are Trigger Points?
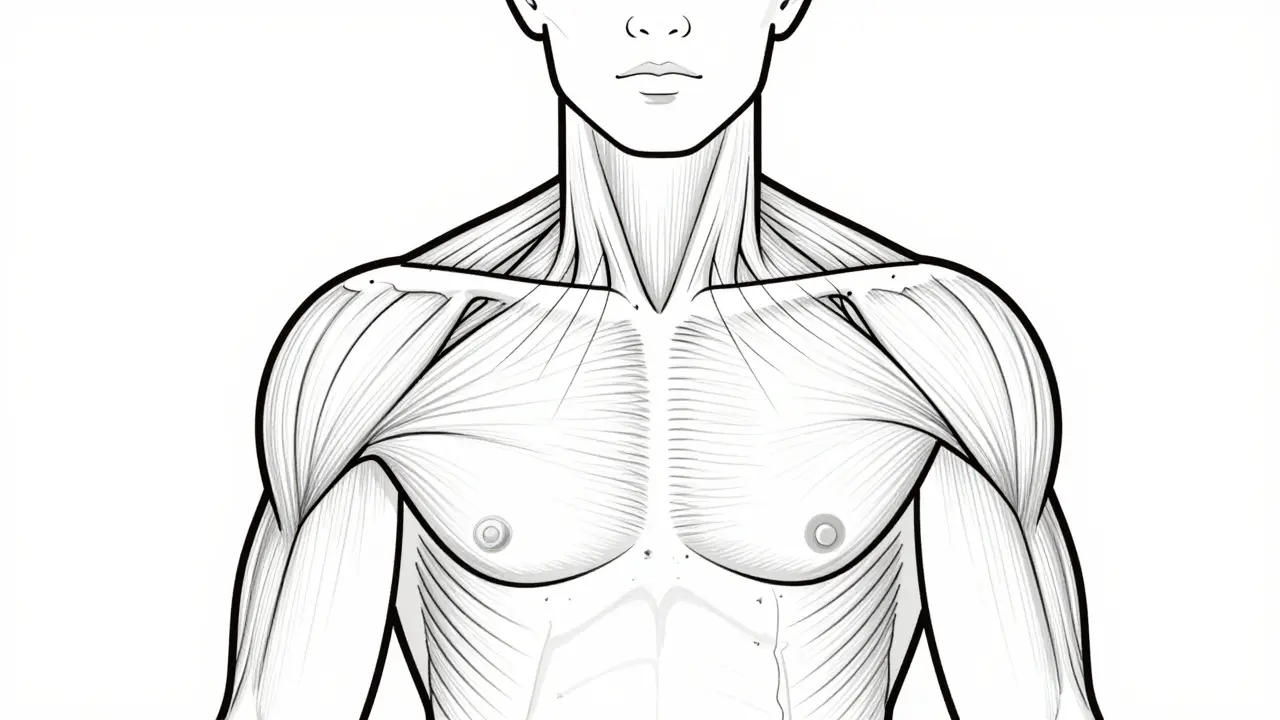
Trigger points aren’t just tender spots. They’re hyperirritable bands of muscle tissue, usually about the size of a pea or a small grape. You can feel them as hard lumps under your skin, often in the upper back, neck, shoulders, or jaw. Press on one, and it doesn’t just hurt where you touch it - it sends pain elsewhere. That’s called referred pain. A trigger point in your trapezius muscle (the big muscle from your neck to your shoulder) can make your forehead throb. One in your jaw muscle can mimic a toothache. These knots form because muscle fibers get stuck in a constant state of contraction. Think of it like a tiny cramp that never releases. The area becomes low on oxygen, acidic, and flooded with pain-signaling chemicals like acetylcholine and serotonin. This creates a loop: pain causes more muscle tightness, which causes more pain. It’s the pain-spasm-pain cycle. There are two types: active and latent. Active trigger points hurt all the time - even when you’re not touching them. Latent ones only hurt when pressed. But both can limit movement, weaken muscles, and mess with your posture over time.How Is It Different From Fibromyalgia?
People often confuse myofascial pain syndrome with fibromyalgia. They’re not the same. Fibromyalgia causes widespread, symmetric pain all over the body - usually in specific tender points that hurt only when pressed, with no referred pain. Myofascial pain is localized to specific muscles and follows predictable referral patterns. One trigger point in your levator scapulae (the muscle that lifts your shoulder blade) will always refer pain to the side of your neck and behind your ear. That’s consistent. Fibromyalgia doesn’t work like that. Also, fibromyalgia often comes with fatigue, sleep issues, and brain fog. Myofascial pain is mostly about muscle pain and movement restrictions. If your pain is only in one area, and it moves in a pattern, it’s likely MPS.Why Do Trigger Points Form?
It’s not just from overdoing it at the gym. Trigger points develop from a mix of factors:- Posture: Sitting hunched over a desk for hours? That’s a recipe for trigger points in your upper traps and levator scapulae. Forward head posture increases their likelihood by 3 to 5 times.
- Trauma: Whiplash from a car accident? Up to 70% of people develop trigger points in the neck and shoulders after that.
- Imbalances: A leg length difference of more than a centimeter can throw off your pelvis and spine, causing trigger points in your glutes, lower back, or even calves.
- Nutrition: Low vitamin D (under 20 ng/mL) is linked to a 60% higher chance of developing MPS. Hypothyroidism is also common in chronic cases.
- Stress: When you’re tense, your muscles stay tight. That constant clenching - especially in the jaw, neck, and shoulders - builds trigger points over time.
How Do You Know If You Have Them?
A trained professional can diagnose trigger points using four key signs:- A taut band you can feel in the muscle - like a tight rope under your skin.
- Local tenderness when you press on it.
- Referred pain that matches known patterns (like pain from your shoulder blade radiating down your arm).
- A local twitch response - when the muscle jumps or twitches as you press on the trigger point. This happens in 70-85% of active trigger points.
Release Techniques That Actually Work
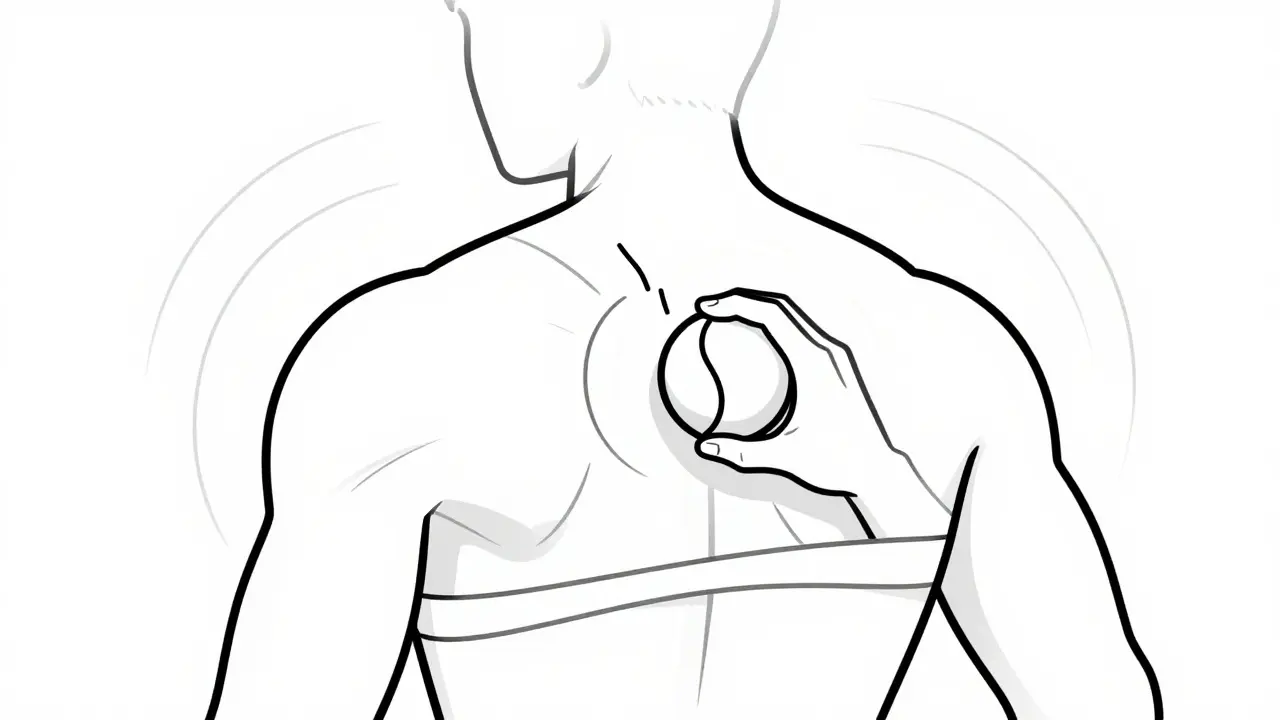
There’s no one-size-fits-all fix, but several techniques have solid evidence behind them.Ischemic Compression
This is the most accessible method. You apply steady pressure - with your fingers, a tennis ball, or a foam roller - directly on the trigger point. Hold it for 30 to 90 seconds until the pain eases by about half. Then release. Repeat 2-3 times. Do this daily. Studies show 60-75% of people get short-term relief. It’s simple, cheap, and you can do it at home.Dry Needling
This is when a physical therapist or trained provider inserts thin needles into the trigger point - no medicine, just the needle. The goal is to get that local twitch response. When it happens, the muscle releases. Pain relief often lasts 4 to 12 weeks. Research shows 65-80% of patients benefit. It’s not needles for acupuncture - it’s targeted muscle work. You might feel a brief cramp or zap during the twitch. That’s normal.Trigger Point Injections
A local anesthetic like lidocaine is injected directly into the trigger point. It gives immediate relief in 70-85% of cases. But here’s the twist: studies show it’s no more effective than dry needling at 4 weeks. The benefit is faster relief, especially for severe pain. Insurance often covers it if other methods fail.Spray and Stretch
A cooling spray (like ethyl chloride) is sprayed over the area where the pain is referred. Then the muscle is gently stretched. The cold helps reduce pain signals, making the stretch more effective. It’s commonly used for neck and jaw pain. Success rates are around 50-65%.Instrument-Assisted Soft Tissue Mobilization (IASTM)
Tools like stainless steel or plastic scrapers are used to glide over the tight muscle. It breaks up adhesions and improves blood flow. It’s popular among athletes and physical therapists. Works well in combination with stretching.Low-Level Laser Therapy (LLLT)
A non-invasive option using specific wavelengths of light. It reduces inflammation and may help reset muscle function. Results are slower - you need multiple sessions - but it’s good for people who can’t tolerate pressure or needles.What Doesn’t Work (and Why)
Not all treatments are equal. Massage alone, if it’s just general relaxation, rarely helps. Trigger points need targeted pressure. Chiropractic adjustments without addressing the muscle knots? Usually not enough. Painkillers like ibuprofen might reduce inflammation, but they don’t fix the muscle contraction. And here’s a big one: if your provider doesn’t know the exact referral patterns or can’t find the taut band and twitch response, they’re not treating trigger points - they’re guessing. That’s why some people say, “I tried everything and nothing worked.” It’s not that the techniques don’t work - it’s that they weren’t done right.Home Care: What You Can Do Daily
The best results come from combining professional care with daily self-management:- Self-compression: Use a tennis ball against a wall or the floor. Roll slowly over the tight area. Don’t rush. Spend 15-20 minutes a day.
- Heat before stretching: Apply a warm towel or heating pad (40-45°C) for 15 minutes before stretching. Heat loosens the muscle.
- Stretching: Hold each stretch for 30 seconds. Repeat 3 times. Focus on the muscles that refer pain - upper traps, levator scapulae, pecs, jaw muscles.
- Posture: Sit back in your chair. Keep your screen at eye level. Avoid cradling your phone between ear and shoulder.
- Check your vitamin D: Get tested if you’re tired, sore, and not improving. Many people with chronic pain are deficient.

Why It Keeps Coming Back
Even after relief, 40-60% of people see symptoms return within 6 months. Why? Because the root cause wasn’t fixed. If you keep slouching at your desk, if your leg length difference goes uncorrected, if you keep clenching your jaw during stress - the trigger points will return. MPS isn’t a one-time fix. It’s a management condition. Like high blood pressure, you need ongoing habits to keep it under control.When to See a Professional
If you’ve tried self-care for 4-6 weeks with no improvement, it’s time. Look for a physical therapist, osteopath, or doctor trained in trigger point therapy. Ask if they use the twitch response and referral patterns in their diagnosis. Avoid anyone who treats you with generic massage or just “cracks your back.” The American Academy of Physical Medicine and Rehabilitation offers certification for providers. That’s a good sign they know what they’re doing.The Bigger Picture
Myofascial pain syndrome is one of the most common reasons people end up with unnecessary MRIs, nerve conduction tests, or even surgery - because no one looked at the muscles. It’s estimated that 30% of all musculoskeletal visits in primary care are due to trigger points. With the opioid crisis pushing doctors toward non-drug pain solutions, trigger point therapy is becoming more mainstream. It’s safe, low-cost, and effective when done right. It’s not magic. It’s mechanics. Your muscles aren’t broken. They’re stuck. And with the right pressure, patience, and persistence, they can learn to let go.Can trigger points cause headaches?
Yes. Trigger points in the upper trapezius, levator scapulae, and temporalis muscles are common causes of tension-type headaches and even migraines. The pain often starts at the base of the skull and radiates to the forehead or behind the eyes. Many people who think they have chronic migraines actually have myofascial pain triggering the symptoms.
Is dry needling the same as acupuncture?
No. Acupuncture is based on traditional Chinese medicine and targets energy meridians. Dry needling is grounded in Western anatomy and targets specific muscle trigger points. The needles are the same, but the technique, location, and purpose are completely different. Dry needling aims to get a local twitch response - acupuncture does not.
How long does it take to see results from trigger point release?
Some people feel relief after one session, especially with dry needling or injections. For most, noticeable improvement takes 2-4 sessions over 2-3 weeks. Long-term results depend on combining treatment with daily self-care like stretching and posture correction. Pain relief typically lasts 4-12 weeks, but recurrence is common without ongoing maintenance.
Can I use a foam roller for trigger points?
Yes, but only if you target the right spot. Rolling over a large muscle group won’t help. You need to find the tight band - the hard knot - and press directly on it. Use a tennis ball for precision. Foam rollers are better for general muscle relaxation. For trigger points, small, focused pressure works better than broad rolling.
Why do some people say trigger points aren’t real?
Some scientists argue that trigger points aren’t visible on imaging scans and lack a single biological marker. But that doesn’t mean they’re not real. Many pain conditions - like fibromyalgia - also lack clear imaging proof, yet they’re accepted clinically. The key is consistency: trigger points produce predictable referred pain patterns, respond to specific pressure, and improve with targeted treatment. Thousands of patients get relief every day - that’s clinical evidence.
Should I get a massage or see a physical therapist?
A general massage may feel good, but it won’t fix trigger points. You need someone trained in myofascial release who can locate taut bands, reproduce referred pain, and elicit a twitch response. Look for a physical therapist, osteopath, or chiropractor with specific training in trigger point therapy. Ask about their experience with Travell and Simons’ referral patterns.



8 Comments
This post is just a long-winded ad for dry needling and trigger point injections. I've had chronic back pain for years and tried all this stuff. Most of it is placebo. The real fix? Stop sitting like a lump and get a better chair. No magic knots, just bad habits.
Also, vitamin D? Please. I took 5000 IU daily for a year and still hurt. Coincidence isn't causation.
As an American physical therapist with 22 years of clinical experience, I must emphasize that the American Academy of Physical Medicine and Rehabilitation's guidelines are unequivocal on this matter. The concept of trigger points, while popularized by Travell and Simons, lacks robust, reproducible biomechanical evidence under double-blind conditions. The so-called 'twitch response' is likely a reflexive neuromuscular artifact, not a therapeutic indicator. Furthermore, the statistical claims in this post-60-75% relief, 65-80% benefit-are not derived from longitudinal, peer-reviewed RCTs but from small, industry-funded pilot studies. This is pseudoscience dressed in medical jargon, and it undermines legitimate pain management protocols.
What if the trigger point isn't the problem but the symptom? We treat the knot like it's the enemy, but what if the knot is the body's desperate attempt to stabilize a broken system? A misaligned pelvis. A leaky gut. A nervous system stuck in fight-or-flight. We squeeze the muscle like it's a water balloon hoping the pressure will go away-but the pressure is the message.
Maybe the trigger point is the soul of the muscle screaming, 'I'm not the issue, I'm the messenger.'
And if you're not asking why your body built this knot in the first place-you're just rearranging deck chairs on the Titanic.
I've been dealing with this for years after my car accident. The trigger point in my levator scapulae was making my whole left side feel like it was in a vice. Tried massage, acupuncture, even chiropractic-nothing stuck until I started using a lacrosse ball against the wall every night for 10 minutes. Took 3 weeks but now I can turn my head without wincing.
Also, got my vitamin D checked-was at 18 ng/mL. After 3 months of supplementation, the morning stiffness dropped by half. It's not magic, but it works if you stick with it.
And yeah, foam rollers are useless for this. Need something small and hard. Tennis ball, lacrosse ball, even a water bottle if you're desperate.
trigger points r a gov mind control tool 2 make ppl buy expensive needles n avoid the real cause: 5g radiation from cell towers makin muscles spasm!!1!1! i had a headache for 3 months n my physio said 'dry needling' but i knew better-i wore a tin foil hat n drank apple cider vinegar n poof! gone. also vitamin d is a lie. its fluoride in the water that makes u feel sore. 🤫💊👁️🗨️
Just wanted to say thank you for this post. I’ve been struggling with tension headaches for years and thought I had migraines. Turns out, it was trigger points in my temporalis and upper traps. Started doing daily self-compression with a tennis ball and stretching-only 15 minutes a day-and within 3 weeks, my headaches dropped from daily to once a week.
It’s not glamorous, but it’s real. I wish I’d known this 5 years ago.
Also, if you’re reading this and skeptical-try it for 2 weeks. No cost, no risk. Worst case? You get a nice shoulder massage. Best case? You never have to take another ibuprofen again. 💪
I appreciate the thoroughness of this post. The distinction between myofascial pain syndrome and fibromyalgia is critical and often misunderstood in clinical practice. I’ve seen multiple patients misdiagnosed with fibromyalgia when their symptoms were clearly localized and referral-pattern-dependent.
One point to add: the role of sleep quality cannot be overstated. Poor sleep increases sympathetic tone, which exacerbates muscle hypertonicity and impairs tissue recovery. Even if trigger point therapy is applied correctly, without addressing sleep architecture, recurrence is nearly inevitable.
Also, thank you for emphasizing that general massage is insufficient. Precision matters. This deserves more attention in primary care.
So you're telling me the body has little knots that cause pain and you can fix them by poking them with a ball or a needle
Wow
Next you'll say the soul is a muscle and you can stretch it with yoga
Everything is just mechanics now
Nothing is spiritual
Nothing is energy
Just little balls of tension in your trapezius
How convenient for the physical therapy industry
What about the meaning of pain
What about the soul's resistance to modern life
Why do you reduce everything to physics
Why are you so afraid of mystery