
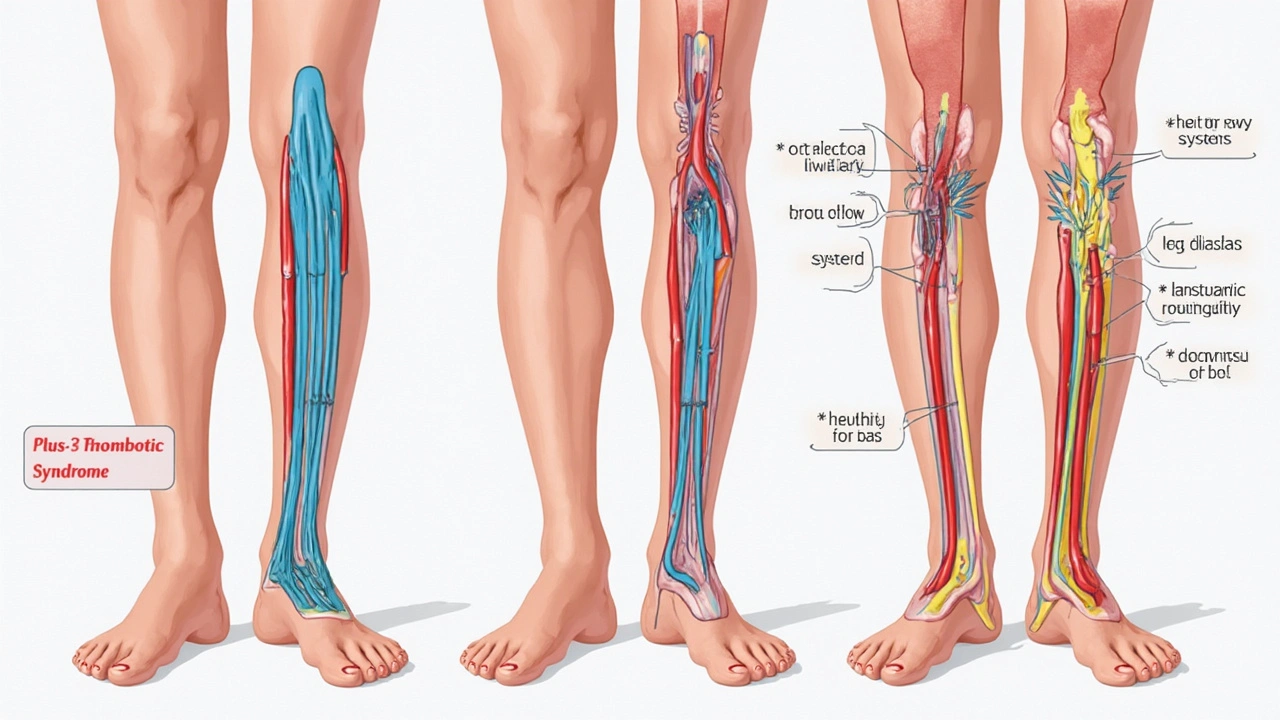
It’s wild how something that happens deep inside your body—way down in your leg veins—can come back to haunt you long after you think you’re in the clear. If you’ve heard of deep vein thrombosis (DVT), you probably know it’s a blood clot that forms in the legs, usually after sitting too long, surgery, or an injury. But there’s a sneaky sidekick too many folks don’t know about: post-thrombotic syndrome (PTS). This thing turns the relief of beating DVT into months or years of dealing with swelling, aching, and changes that mess with everyday life.
What Post-Thrombotic Syndrome Really Means For Life After DVT
Let’s picture it: you survived a blood clot. The hospital visits, the scary words, the blood thinners—all done. You think you’re safe. But then, weeks or even years later, that same leg starts to puff up after a bit of walking, or you spot reddish skin and weird pain that leaves you frustrated and confused. That’s PTS poking its head out. It’s a chronic condition, not just a passing nuisance. Doctors estimate about 20% to 50% of people who get a DVT in their leg will develop some degree of post-thrombotic syndrome. Not exactly rare.
Why does this happen? When a DVT forms, the blood clot causes a traffic jam in the vein. Even after you clear the blockade, leftover damage to the valves in your veins or permanent narrowing keeps blood from flowing the way it should. Your veins are like a two-way road that suddenly loses its lane dividers—chaos follows. Healthy valves keep blood moving up, but damaged ones let some of it trickle back down, pooling in the lower parts of the leg. That’s where all the classic PTS trouble starts: heavy legs, throbbing pain, swelling (often getting worse as the day goes on or after lots of standing), and weird skin changes like hardening or dark patches. Some people even develop open wounds, called ulcers, which are stubborn to heal and sometimes lead to infections.
Ever wonder if you’re in the risk group? Some clear triggers dial up the odds. Big risk boosters include having a large blood clot that stretches from the calf all the way up near the thigh or groin, being overweight, being older, or suffering more than once from DVT in the same spot. Folks who skip or stop anticoagulant medication early (those blood thinners you hated taking) are playing with fire. Sitting for hours—as you might when driving across New Zealand or flying to Oz—levels up your risk, but so does not moving at all after an injury or surgery.
A study out of Europe in 2023 followed DVT patients for three years. Shockingly, 40 percent developed signs of PTS, and roughly one in ten had severe symptoms interfering with their jobs and day-to-day stuff like going grocery shopping or even taking a stroll on Takapuna Beach. So if you thought DVT was just a one-off health scare, PTS might try to prove you wrong.
Recognising Post-Thrombotic Syndrome: No, It’s Not Just "Getting Older"
How do you know it’s PTS and not just a rough gym session or too much time on your feet? The telltale signs are relentless swelling—usually starting by the ankle, then rising up the leg as the day wears on. You might catch yourself absentmindedly rubbing your calf or ankle, feeling that tightness and mild to moderate pain that just won’t quit. Your skin may take on a brownish tinge or seem thin and fragile, especially on the shin. In the worst cases, you could notice ulcers or sores that pop up around the ankle or lower leg. They’re not pretty, and they don’t heal quickly.
Here’s a simple breakdown of classic PTS symptoms:
- Chronic leg swelling (often worse by evening)
- Aching, heaviness, or cramps—especially after standing or walking
- Itching or tingling skin
- Red or brown spots and hardened, thick skin
- Small or large ulcers near the ankle
It’s easy for people to brush off leg changes as just “part of getting older” or “that’s what happens after an injury.” But these symptoms should make you pause, and if you’ve had a DVT, your GP or a vein specialist needs to know. There’s even a PTS scoring chart called the Villalta scale that doctors use. They score pain, swelling, and skin changes from mild to severe—scores over 5 usually mean PTS.
Not every discomfort after a DVT is post-thrombotic syndrome. Muscular aches clear up with rest. Swelling from a temporary injury fades. PTS sticks around for months or gets worse over time, especially if nothing’s done.
Women often notice changes first, possibly because the swelling and skin changes play havoc with shoes or tights. Men tend to dismiss symptoms—"it’s just a sports niggle." Don’t do that; early recognition means treatment can actually do something.
Your day-to-day doesn’t have to revolve around PTS, but ignoring these signs makes you more likely to face things like chronic ulcers. An Auckland review from late 2022 found Kiwis with untreated moderate-to-severe PTS lost an average of 8 to 12 days of work every year, mostly from infections or pain that made walking a nightmare.
| Symptom | Incidence (%) |
|---|---|
| Leg Swelling | 72 |
| Pain or Heaviness | 65 |
| Skin Colour Changes | 42 |
| Skin Thickening | 34 |
| Ulcer Formation | 11 |

Practical Strategies for Managing and Reducing the Impact of PTS
Let’s get into what actually helps—not just for surviving post-thrombotic syndrome, but for getting your life (and legs) back. First off, don’t believe there’s no hope. There are ways to rein in the misery, and most of them don’t require fancy equipment or endless trips to specialists. Consistency and lifestyle tweaks make the real difference.
Compression stockings are the gold standard. Yes, they’re not a fashion statement. But the difference between wearing these regularly and not is like night and day. Graduated stockings—meaning tightest at the ankle, looser up top—help push blood upwards, fighting that pooling effect. Most doctors in New Zealand prescribe 20-30 mmHg compression, and you can get them fitted at the chemist. Some users report improvement in swelling, skin quality, and stamina within a few weeks. Just make sure to put them on first thing in the morning before getting out of bed. (If you wait until you’re upright, swelling can start before the stockings go on.)
Movement is critical. Long stretches sitting at a work desk or binge-watching Netflix only fuels the fire. Get up every hour, walk around, and flex your ankles. Leg elevation is another biggie—prop your feet up on the couch or a chair whenever you can, especially after a long day on your feet. It’s not lazy; it literally helps the body fight gravity and decrease swelling. Some folks even keep a footstool under their desk for this reason.
Watch your weight. If you’re carrying extra kilos, it puts even more pressure on the veins and multiplies damage from PTS. In New Zealand, nearly one in three adults are overweight—so you’re far from alone if this is a battle for you. Dropping weight, even just five to ten percent of your body mass, lets veins recover and may lessen achiness and inflammation.
Good skin care shouldn’t be underestimated. PTS makes skin fragile, prone to itching, and at real risk for ulcers. Use mild soaps, moisturise daily, and check your lower legs regularly for new spots, cuts, or changes. If an ulcer starts—no matter how tiny—see your GP or wound nurse right away. Early wounds heal far better than the big, chronic ones.
There are a few more practical tools and everyday hacks:
- Stay hydrated: Blood flows better when you drink enough water.
- Wear loose, comfortable shoes; avoid high heels or tight boots.
- Don’t cross your legs for long periods (it slows venous return).
- If you smoke, quit—smoking damages blood vessels and slows healing.
- Get moving: cycling and swimming benefit circulation with less joint pressure.
Anticoagulants, if still prescribed, are crucial. Stick to your medication and don’t skip doses. Regular check-ups matter: your health team keeps tabs on new symptoms or potential complications. Don’t be shy about reporting pain or swelling, even if you think it’s minor or they’ve “heard it before.”
Even with careful management, watch for warning signs that call for immediate action: sudden dramatic swelling, new redness, fever, or pain that’s way outside your usual. These can signal a new DVT or infection. Fast action means fewer problems down the line.
Sometimes, the basic stuff isn’t enough. Severe cases (about 5-10% of PTS sufferers) may benefit from vein procedures, like angioplasty or surgery, especially if ulcers don’t heal or pain limits your daily life. Most people never need these, but it’s good to know they exist—and they’re far better when caught early than after months of misery.
PTS shouldn’t stop you from travelling, exercising, or enjoying life in Auckland (or wherever fate takes you). It means listening to your body, staying on top of symptoms, and using the small but powerful tools medical science offers. If you stay proactive—literally on your toes—PTS becomes a manageable twist on the DVT story, not the ending.




14 Comments
So basically your veins just give up and start a protest. No warning. No fanfare. Just swelling like you’re slowly turning into a balloon. And the worst part? You thought you were done. Nope. Your body’s like, ‘lol, let’s make this a sequel.’
The pathophysiology is straightforward: venous valve endothelial disruption leads to retrograde flow and increased hydrostatic pressure, resulting in chronic venous hypertension. The 2023 EU/PTNZ data shows a 40% incidence rate, which aligns with meta-analyses from the Journal of Vascular Surgery. But nobody talks about the biomechanical inefficiency of compression stockings-70% of patients don’t wear them correctly due to improper fit and lack of patient education.
Bruh… I had a DVT in 2020 and I still wear compression socks like they’re part of my soul. But also, I’m not even mad. 😅 Life’s just weird like that. You survive the clot, then your leg becomes a haunted house. But hey, at least I don’t have ulcers. Yet.
I appreciate the thoroughness of this post. It is imperative to recognize that post-thrombotic syndrome is not merely a consequence of DVT, but a chronic venous disorder requiring longitudinal management. The Villalta scale, as referenced, is a validated instrument and should be routinely employed in follow-up protocols. Furthermore, adherence to anticoagulation therapy remains the most critical modifiable factor in reducing incidence.
You got this. Compression socks are annoying but they’re your new best friend. Get up every hour. Elevate when you can. Drink water. Don’t ignore the little stuff. You’re not broken-you’re just learning a new way to move through the world. One step at a time.
The clinical evidence supporting graduated compression therapy (20–30 mmHg) is robust. Studies demonstrate a 50% reduction in PTS progression with consistent use. Additionally, weight loss of ≥5% body mass significantly improves venous return. It is essential to differentiate PTS from acute musculoskeletal pain; persistent edema beyond six weeks post-DVT warrants vascular referral.
I remember the first time I noticed it-my ankle looked like a deflated balloon someone had stuffed with sand. I thought it was just my shoes. Then the skin turned brown. Then the itching. Then the shame. I stopped wearing shorts. I stopped going to the beach. I stopped telling people why I was always sitting down. It’s not just a symptom. It’s a whole new identity. And no one talks about that part. The loneliness. The quiet grief of your body betraying you after you thought you’d won.
One thing I’ve learned from working with PTS patients: consistency beats intensity. You don’t need to run marathons. Just walk 10 minutes every couple hours. Elevate while you watch TV. Put on those socks before your feet hit the floor. Tiny habits, massive impact. You’re not failing-you’re just in the long game.
Your legs are not your enemy. They’re just holding onto trauma. Think of compression socks as hugging your veins back into shape. Move like you mean it. Hydrate like your life depends on it-because it kinda does. And if your skin starts acting weird? Treat it like a crying baby. Gentle. Patient. No judgment. You’ve survived the clot. Now let’s survive the aftermath-with style.
The prevalence figures cited are consistent with published epidemiological data. However, the assertion that PTS is underdiagnosed due to patient dismissal of symptoms lacks empirical validation in the referenced study. Further, the recommendation to avoid high heels is anecdotal and not supported by controlled trials.
You people treat this like it’s a wellness blog. It’s venous insufficiency. It’s a medical condition. Stop romanticizing compression socks like they’re yoga pants. If you’re not on anticoagulants or seeing a vascular specialist, you’re just doing TikTok medicine.
So my leg is basically a slow-mo horror movie and I’m the star? 🙃 At least I don’t have to worry about fashion anymore. Compression socks are my new power suit. 🖤
This is an exceptionally well-researched and clinically grounded summary. I would only add that early intervention with supervised exercise therapy and pneumatic compression devices in high-risk patients may further reduce the incidence of ulceration. Multidisciplinary care is paramount.
I’ve been living with PTS for 7 years. I used to hate my legs. Now I thank them. They carried me through chemo, surgery, grief, and 3 cross-country moves. Yeah, they ache. Yeah, they look weird. But they’re still here. And so am I. Wear the socks. Move. Cry if you need to. Then get up and walk again.