Getting vaccinated while on immunosuppressants isn’t just about showing up at the clinic. It’s about timing-and getting it wrong can mean the difference between protection and vulnerability. If you’re taking drugs like rituximab, methotrexate, or azathioprine for autoimmune disease, cancer, or organ transplant, your immune system is already working under heavy restrictions. Vaccines? They need a fighting chance. And that means planning, not guessing.
Why Timing Matters More Than You Think
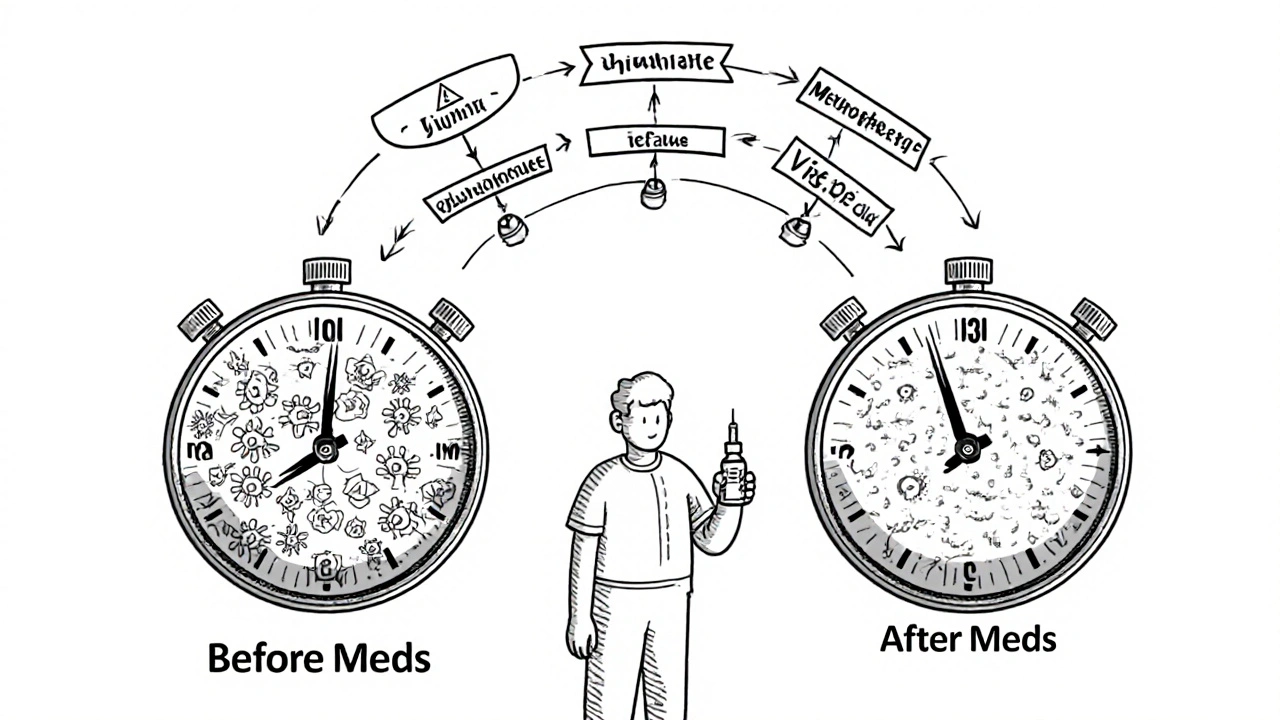
Your body doesn’t respond to vaccines the same way when immunosuppressants are active. These drugs are designed to quiet your immune system-so when you get a vaccine, your body might not make enough antibodies. That’s not just a theory. Studies show people on rituximab can have up to 80% lower antibody response to COVID-19 vaccines if vaccinated too soon after treatment. The same goes for flu and shingles shots. The CDC, ACR, and IDSA all agree: if you want protection, you need to time it right.When to Vaccinate Before Starting Immunosuppressants
The safest window is before you even start your medication. Most guidelines say: get your vaccines at least 14 days before beginning immunosuppressants. Some experts push for 2 to 4 weeks, especially for live vaccines like shingles or nasal flu. Why? Because your immune system still has its full strength before the drugs kick in. Once you start, your ability to respond drops fast. For example, if you’re about to begin methotrexate for rheumatoid arthritis, get your flu shot two weeks before your first dose. If you’re starting rituximab for lupus or lymphoma, aim for at least four weeks before. Some specialists recommend waiting six months after a full course of rituximab before getting non-flu vaccines-because B-cells take that long to come back.What Happens If You’re Already on Medication?
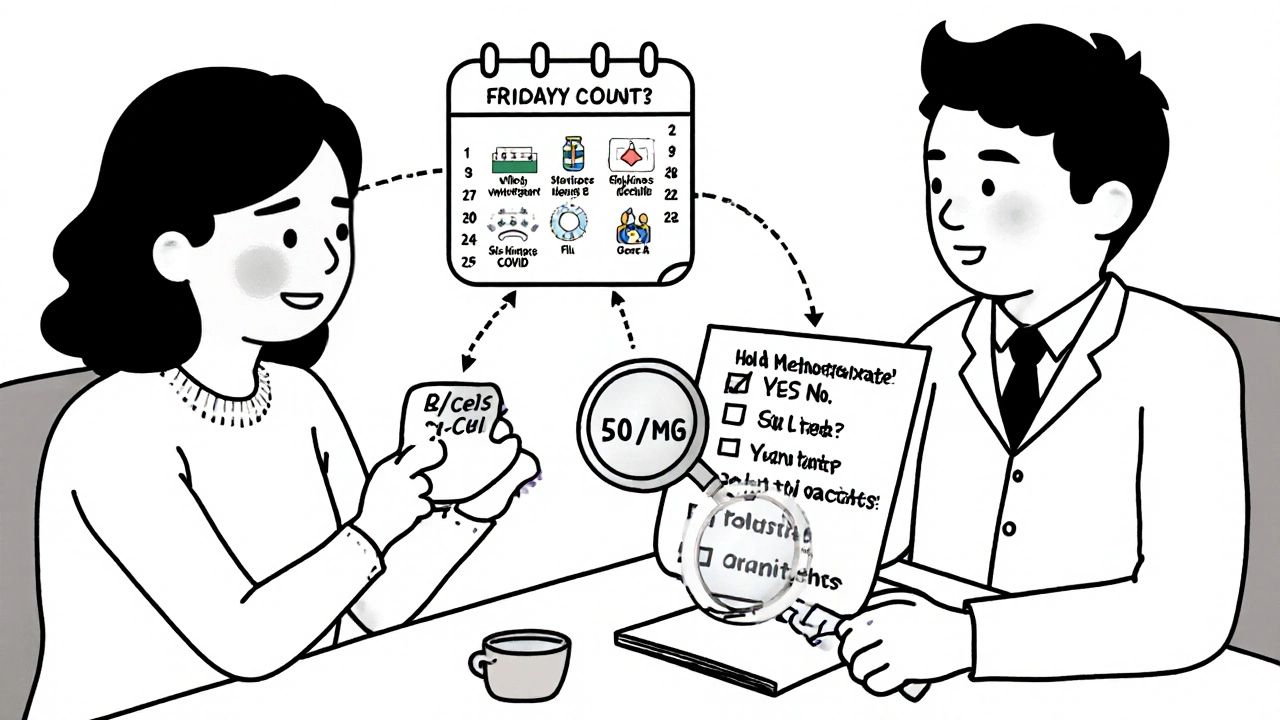
If you’re already on immunosuppressants, don’t panic-but don’t assume vaccines won’t work either. They might be less effective, but they’re still better than nothing. The key is adjusting your meds around the shot. Here’s what the major guidelines say for common drugs:- Methotrexate: Hold for two weeks after your flu shot if your disease is stable. This isn’t just advice-it’s backed by trials showing a 27% increase in antibody production.
- Rituximab: Wait at least six months after your last dose before getting shingles, pneumococcal, or hepatitis B vaccines. For flu, some experts say you can go earlier if community transmission is high, but most stick to the six-month rule.
- TNF inhibitors (like Humira or Enbrel): Skip one dose before vaccination, then wait four weeks before restarting.
- Azathioprine, mycophenolate, cyclophosphamide: You can usually keep taking these for inactivated vaccines (like flu or COVID). But if you’re getting a live vaccine, stop for four weeks before and after.
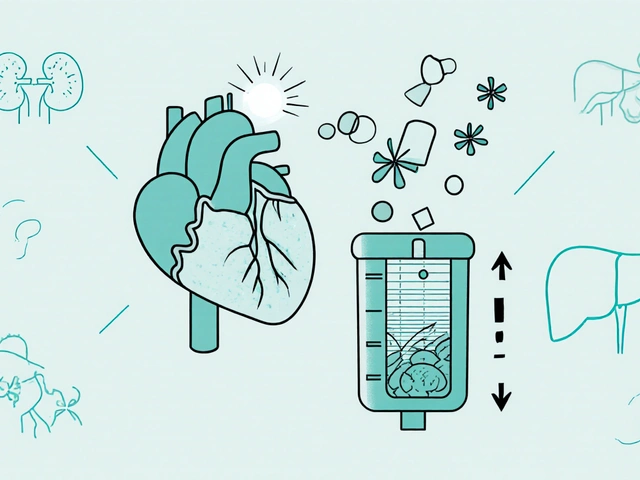
- IVIG (intravenous immunoglobulin): This one’s tricky. If you get 1 gram per kg, you need to wait 10 months before a live vaccine. After the shot, hold off for four weeks. Why? IVIG contains antibodies that can neutralize the vaccine.
Contradictions Between Guidelines
Not all experts agree. The CDC says 14 days before therapy is enough. The American Society of Hematology says 2-4 weeks. The ACR says six months for rituximab. The European League Against Rheumatism says 7-10 days is fine for biologics. These differences aren’t just academic-they affect real decisions. A 2023 survey in the Journal of Rheumatology found 68% of rheumatologists felt confused by the conflicting advice. One patient in Boston waited six months for a shingles vaccine after rituximab-and still got shingles. Another in Seattle got her flu shot three weeks before starting methotrexate and never got sick. Timing matters. But so does context.Real-World Problems: Delays, Flares, and Missed Shots
It’s not just about the science. It’s about logistics. At Massachusetts General Hospital, 42% of patients on rituximab had their vaccines delayed past the six-month window. Eighteen percent got sick during that gap. At the same time, 31% of patients who paused their meds to get vaccinated had disease flares. One woman with lupus had a kidney flare after stopping mycophenolate for two weeks. She ended up in the hospital. Primary care doctors often don’t know the rules. A 2023 survey found 47% of family physicians struggled to get clear guidance from specialists. Patients are left guessing. Reddit threads are full of frustration: “I waited six months and got shingles anyway. My doctor said it was unavoidable.”What’s Changing: The Future of Personalized Timing
The old model-fixed time intervals-is falling apart. Experts now say: measure your immune system, not just the calendar. The IDSA’s 2025 draft guidelines recommend checking B-cell counts before vaccination. If your count is above 50 cells/μL, you’re likely ready. That’s more accurate than waiting six months blindly. The NIH is running a study called VAXIMMUNE, tracking 2,500 patients to see if immune biomarkers can replace fixed schedules. Even tech is catching up. Epic Systems, the biggest electronic health record company, is rolling out a vaccine timing tool in 2025. It will auto-calculate your window based on your meds, dose, and local disease risk. No more spreadsheets or manual calculations.What You Should Do Right Now
If you’re on immunosuppressants:- Make a list of every medication you take-including doses and last administration date.
- Know which vaccines you need: flu, COVID, shingles, pneumococcal, hepatitis B, tetanus.
- Ask your doctor: “Which of my meds need to be held, and for how long?” Don’t assume.
- If you’re getting a live vaccine (like shingles), confirm whether it’s safe with your current meds.
- Ask about antibody testing after vaccination. Some clinics now offer it to check if the vaccine worked.
Final Thought: Protection Isn’t One-Size-Fits-All
There’s no perfect answer. But there’s a better way than waiting for illness to strike. The goal isn’t just to get a shot-it’s to get the right shot at the right time. For some, that’s two weeks before starting methotrexate. For others, it’s waiting for B-cells to rebound. For everyone, it’s asking the right questions. Don’t let confusion cost you your health.Can I get the flu shot while on methotrexate?
Yes, but you’ll get a stronger response if you hold methotrexate for two weeks after the shot. Studies show this increases antibody production by 27%. If your disease is active, talk to your doctor-sometimes it’s safer to keep taking it. The flu shot is inactivated, so it’s safe to use while on methotrexate.
How long after rituximab can I get the shingles vaccine?
Wait at least six months after your last rituximab dose. The shingles vaccine is live, and your B-cells need time to recover. Some guidelines say you can get it as early as three months if your immune system is recovering well, but most specialists stick to six months to be safe. Getting it too soon means the vaccine won’t work.
Do I need to stop my biologics before a COVID vaccine?
For TNF inhibitors like Humira or Enbrel, hold one dose before the shot and wait four weeks before restarting. For other biologics like abatacept or tocilizumab, timing isn’t as clear. Some experts recommend holding, others don’t. Ask your rheumatologist. For most people, getting the vaccine on time is more important than holding meds-unless you’re on rituximab.
Is it safe to get vaccines while on IVIG?
It depends on the dose. If you get 1 gram per kg of IVIG, wait 10 months before a live vaccine like shingles. After the shot, wait four weeks before your next IVIG dose. IVIG contains antibodies that can block the vaccine. For inactivated vaccines like flu or COVID, you can usually get them without delay, but effectiveness may be reduced.
Can I get vaccinated during a disease flare?
Generally, no. Vaccines are safest when your condition is stable. If you’re having a flare, your immune system is already overworked. Delay the shot until your symptoms improve. If you’re on high-dose steroids, wait until you’re on a lower dose. Your doctor may adjust your meds to create a window for vaccination.
Should I get antibody tests after vaccination?
It’s not routine, but it’s worth asking. Some clinics now offer antibody tests for COVID, flu, and hepatitis B after vaccination in immunosuppressed patients. If your levels are low, you may need a booster or additional doses. This is especially helpful if you’re on rituximab or high-dose steroids.



14 Comments
The CDC's 14-day window is a bare minimum. If you're on rituximab, waiting six months isn't overcautious-it's medically necessary. I've seen patients get flu shots at 90 days post-treatment and still seroconvert at 5% efficacy. That's not protection; that's a false sense of security. Stick to the six-month rule unless you're in a pandemic emergency.
Wait-so we’re supposed to trust guidelines that contradict each other? The ACR says six months, the EULAR says ten days, the CDC says two weeks… Who’s actually in charge here? The pharmaceutical industry? The insurance companies? Someone’s making money off this confusion-and it’s not the patient.
Let me tell you something-this whole system is a circus. I got my shingles shot at five months post-rituximab because my doctor said, ‘It’s better than nothing.’ Guess what? I still got shingles. And now I’m paying $800 a month for nerve pain meds. Meanwhile, my rheumatologist just shrugged and said, ‘We did our best.’ Best? That’s not a medical outcome-that’s a resignation letter.
It's a disgrace that American patients are left to navigate this chaos. In Germany, they have centralized immunosuppressant-vaccine protocols with mandatory specialist coordination. Here? You're lucky if your PCP even knows what methotrexate is. We need federal mandates, not fragmented guidelines from five different societies with conflicting agendas.
In the grand tapestry of human health, we are but threads pulled by the loom of pharmaceutical timelines and bureaucratic indecision. To vaccinate without measuring B-cell recovery is to plant seeds in concrete and call it agriculture. The body does not obey calendars-it obeys biology. And biology, my friends, does not apologize for its patience.
bro i got my flu shot while on methotrexate and didn't hold it and still got sick last year. but this year i held it for 2 weeks after and felt way better. also my doc said if u got a booster after 6 months u get way better response. so yeah its worth it. dont be lazy just ask your rheum.
Dear fellow patient, please do not underestimate the importance of this guidance. Your immune system is not a machine that can be reset with a button. Each medication has a unique biological footprint. Take the time to document your regimen. Consult your specialist. Your life depends on precision-not convenience.
They’re hiding something. Why is IVIG treated like a secret weapon? Why does Big Pharma want us to wait 10 months for live vaccines? It’s not about safety-it’s about profit. If you could get vaccinated right after IVIG, you’d need fewer boosters. Fewer boosters = less revenue. Wake up. The system is rigged. 🤫💉👁️🗨️
Let’s be real-this whole thread is a glorified FAQ. The real problem? Doctors don’t get paid to coordinate vaccines. They get paid to prescribe. So they’ll say ‘it’s fine’ and move on. Your insurance won’t cover antibody testing. Your pharmacy won’t remind you. You’re on your own. And that’s the real scandal.
Thank you for this incredibly thorough breakdown-I’ve been on mycophenolate for 7 years and never knew about the 4-week hold for live vaccines. I got my shingles shot last year without pausing meds and had a mild flare. Now I’m tracking my doses in a spreadsheet with color-coded flags. I even emailed my rheumatologist’s office with a checklist and they sent me a thank-you note. Small changes make a difference. If you’re reading this, please, please ask about antibody testing. It’s not expensive, and it’s life-changing.
Anyone else notice how every single guideline says ‘ask your doctor’ but none of them give you a damn script to take to your doctor? I showed my PCP this post and he said, ‘I’m not a rheumatologist.’ Well thanks for the insight, Captain Obvious. We need a one-pager. A printable cheat sheet. Not another 12-page PDF from the ACR.
It’s not about timing. It’s about surrender. You think holding methotrexate for two weeks will save you? It won’t. You’re still immunocompromised. The vaccine is a placebo wrapped in clinical jargon. The real protection? Avoiding crowds. Wearing masks. Living in fear. That’s what they really want you to do.
I’ve been on Humira for 12 years. I held one dose before my last COVID shot. Felt fine. Got my antibody test back-levels were solid. But here’s what nobody says: your immune system doesn’t forget. Even if the numbers look low, your T-cells remember. You’re not defenseless. You’re just slower. Don’t let the numbers scare you. Stay engaged. Stay informed. And don’t let anyone make you feel guilty for needing help.
As a clinician who works in immunology, I can confirm that the VAXIMMUNE trial is one of the most promising developments in the last decade. Biomarker-guided vaccination will replace arbitrary timelines within five years. The future is personalized, not protocol-driven. Until then, document everything. Bring your medication list. Ask for antibody testing. Advocate. You are not a passive recipient of care-you are the most important variable in the equation.