Weight Gain Risk Calculator for Psychotropic Medications
How Does This Work?
This tool estimates your risk of weight gain based on the medication you're taking and how long you've been on it. Weight gain from psychiatric medications isn't just about willpower—it's biology. Your doctor can help you manage this risk with medication adjustments, lifestyle strategies, and sometimes additional treatments like metformin.
Results will appear here
Why Weight Gain Happens on Psychotropic Medications
It’s not your fault. If you’ve gained weight after starting a new psychiatric medication, you’re not alone-and you’re not lazy. Many antidepressants, antipsychotics, and mood stabilizers directly affect your body’s hunger signals, metabolism, and fat storage. The science is clear: drugs like olanzapine and clozapine can trigger weight gain within weeks. Some people gain 4 to 10 kilograms in the first year, even if they eat the same way they always have.
This isn’t just about appearance. Weight gain from these medications raises your risk for diabetes, high blood pressure, and heart disease. People with serious mental illnesses already live 10 to 20 years less than the general population, and medication-induced metabolic problems are a major reason why. The problem is so common that 30% to 50% of patients on high-risk antipsychotics gain significant weight. The FDA has required metabolic monitoring for these drugs since 2003, and for good reason.
Which Medications Cause the Most Weight Gain?
Not all psychotropic drugs are equal when it comes to weight gain. Some are much worse than others. Among antipsychotics, clozapine and olanzapine are the biggest culprits. Studies show patients on olanzapine gain an average of 4 kg in just 10 weeks. By the end of the first year, it’s not unusual to see 10 kg or more added.
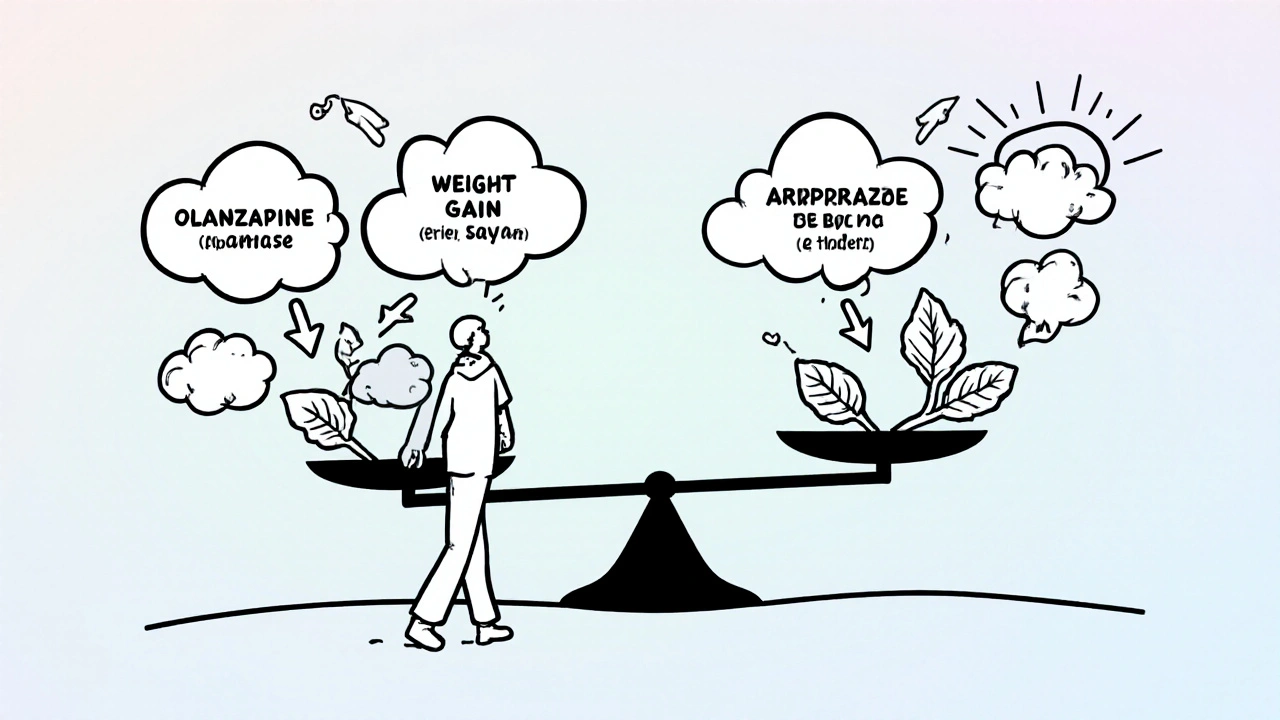
On the other end of the spectrum, lurasidone and aripiprazole cause almost no weight gain. In fact, one study found patients on lurasidone gained just 0.75 kg over a year-compared to 4.15 kg more than those on olanzapine. Paliperidone and asenapine also show minimal effects. If you’re starting a new medication or thinking about switching, this data matters.
Antidepressants aren’t off the hook either. Mirtazapine, amitriptyline, and paroxetine are linked to noticeable weight gain. Even mood stabilizers like lithium and valproate can add pounds. The key takeaway? Your medication choice isn’t just about symptom control-it’s a metabolic decision.
How These Drugs Change Your Body
These medications don’t make you hungry because you’re weak-willed. They change your brain chemistry in ways that directly boost appetite and slow metabolism. The main targets are three receptors: histamine-1, serotonin-2C, and dopamine-2. When these are blocked, your body thinks it’s starving-even when it’s not.
That’s why people on these drugs often crave carbs and sugary snacks. The brain’s reward system gets rewired, making high-calorie foods feel more satisfying. At the same time, insulin resistance can develop, meaning your body stores more fat instead of burning it. Blood sugar, cholesterol, and triglyceride levels often rise, even before the scale moves much. This is called metabolic syndrome-and it’s a silent threat.
And here’s the cruel twist: once you’ve gained weight, it becomes harder to lose. A 2016 study found that people on psychotropic medications lost 1.6% less weight over 12 months than those not on these drugs. Even in structured weight-loss programs, fewer people on psychiatric meds hit the 5% or 10% weight loss targets that improve health outcomes. Your body is fighting you-and it’s not because you’re trying too little.

What You Can Do: Three Proven Strategies
You don’t have to accept weight gain as a side effect you can’t fix. There are three main ways to manage it-and they work best together.
- Switch medications-if your symptoms allow. Moving from olanzapine to aripiprazole or lurasidone can prevent further gain or even lead to weight loss. But don’t do this alone. Stopping or changing psychiatric meds without supervision can trigger relapse. Talk to your psychiatrist about alternatives with lower metabolic risk.
- Add metformin. This diabetes drug has been shown in multiple trials to reduce antipsychotic-induced weight gain by 2 to 4 kg. It helps your body use insulin better, reduces cravings, and can improve cholesterol. It’s not a magic pill, but it’s one of the most studied and safest options.
- Use structured lifestyle support. A dietitian who understands psychiatric meds can help you plan meals that fight cravings without triggering guilt. Exercise doesn’t have to be intense-just consistent. Walking 30 minutes a day, five times a week, improves insulin sensitivity and mood. Programs that combine weekly counseling, meal tracking, and gentle movement have the best results.
Why Most Diets Fail on Psychotropic Medications
Standard weight-loss plans often don’t work for people on these drugs. Why? Because they ignore the biology. A typical low-calorie diet assumes willpower is the main barrier. But if your brain is screaming for carbs due to histamine blockade, willpower isn’t enough.
Successful programs adapt. They don’t just say “eat less.” They say: “Here’s how to eat so your brain doesn’t feel deprived.” That means more protein and fiber to stay full longer. Fewer processed snacks. Planned meals that account for increased appetite. Some patients need to eat more frequently in smaller portions to avoid blood sugar crashes that trigger bingeing.
Exercise is also different. Depression or anxiety might make you feel too tired to move. But low-impact movement-like yoga, swimming, or walking-can help regulate mood and metabolism at the same time. The goal isn’t to burn 500 calories a day. It’s to move consistently so your body doesn’t shut down.
When to Consider Metformin or Topiramate
If you’ve gained more than 7% of your body weight since starting your medication, and lifestyle changes haven’t helped, talk to your doctor about medications that can reverse the trend.
Metformin is the most common choice. It’s affordable, well-tolerated, and backed by solid evidence. Side effects like mild stomach upset usually fade after a few weeks. Many patients report fewer cravings and more energy after starting it.
Topiramate, originally used for seizures and migraines, has also shown promise. Studies show it can lead to 3 to 5 kg of weight loss in people with medication-induced gain. But it can cause brain fog, tingling, or memory issues-side effects that might worsen psychiatric symptoms. It’s not first-line, but for some, the trade-off is worth it.
Emerging options like GLP-1 agonists (e.g., semaglutide) are being studied in psychiatric populations. Early results show 5% to 8% weight loss in small trials. But these are still new, expensive, and not yet approved for this use. For now, metformin remains the most practical option.
Monitoring and Prevention: What Your Doctor Should Be Doing
Weight gain shouldn’t be an afterthought. It should be tracked from day one. The American Psychiatric Association recommends checking weight, waist size, blood pressure, and blood sugar at baseline and every three months after starting a new medication.
Some healthcare systems are leading the way. The Veterans Health Administration has required quarterly metabolic screening for all patients on antipsychotics since 2010. As a result, they’ve improved early detection of problems by 15%. If your provider isn’t doing this, ask why. You deserve proactive care.
Even if you’re feeling stable mentally, ask for a metabolic panel every six months. Many people don’t realize their cholesterol or glucose levels are rising until it’s too late. Catching it early means you can adjust before you need insulin or blood pressure meds.
What’s New: Digital Tools and Genetic Testing
Technology is starting to help. The FDA-cleared Moodivator app, launched in 2021, helps users track food, mood, and movement. In a 2022 trial, users lost 3.2% more weight than those getting standard care. It’s not a replacement for human support, but it’s a useful tool for staying accountable.
On the research front, scientists are looking at genetics. Early studies suggest people with certain variations in the MC4R gene are more likely to gain weight on antipsychotics. In the next few years, genetic testing might help predict who’s at highest risk-so they can start prevention before weight gain begins.
Don’t Stop Your Medication-Work With Your Team
A 2020 survey found that 15% to 20% of people stop taking their antipsychotic meds because of weight gain. That’s dangerous. Relapse can lead to hospitalization, job loss, or worse.
The answer isn’t quitting. It’s partnering with your care team: your psychiatrist, a dietitian who knows psychiatric meds, and maybe a therapist who specializes in body image and behavior change. You’re not fighting this alone. There are tools, medications, and strategies that work.
Weight gain on psychotropic drugs is common. But it’s not inevitable. With the right approach, you can manage your mental health-and your body-at the same time.
Can I lose weight while taking antipsychotics?
Yes, but it’s harder than for people not on these medications. Weight loss requires more structure-like working with a dietitian, using metformin, and sticking to consistent movement. Studies show people on antipsychotics can lose weight, but they need more support and often lose less than those not on meds. Don’t give up-just adjust your strategy.
Which antipsychotic causes the least weight gain?
Lurasidone and aripiprazole cause the least weight gain among second-generation antipsychotics. Lurasidone averages just 0.75 kg of gain over a year-almost the same as placebo. Asenapine and ziprasidone are also low-risk options. If weight is a major concern, ask your doctor if switching to one of these is possible without risking your mental health.
Does metformin help with weight gain from antidepressants?
Yes, though most studies focus on antipsychotics. Metformin improves insulin sensitivity and reduces cravings, which helps with weight gain from any medication that causes metabolic changes-including mirtazapine or paroxetine. It’s not officially approved for this use, but many doctors prescribe it off-label-and it’s been shown to help in real-world cases.
How long does it take to see results from lifestyle changes?
You might notice reduced cravings and more energy in 2 to 4 weeks. But meaningful weight loss-like 5% of your body weight-usually takes 3 to 6 months, especially with medication interference. Patience and consistency matter more than speed. Focus on habits, not the scale.
Should I avoid psychotropic meds because of weight gain risk?
No. These medications save lives and restore functioning for millions. The risk of untreated depression, psychosis, or bipolar disorder is far greater than the risk of weight gain. The goal isn’t to avoid treatment-it’s to choose the safest option and manage side effects early. Work with your doctor to find the right balance.




10 Comments
I gained 20 lbs on olanzapine and felt like a failure until I realized my brain was literally screaming for donuts. Now I eat protein pancakes every morning and it’s a game changer. 🍞😂
This is so real. I was on mirtazapine for 2 years and lost all my confidence. Started metformin and just walked 20 mins a day. Not much but it added up. You’re not broken. Your meds are just being jerks.
Yessss!! Metformin changed my life 🙌 I was gaining 3 lbs a month on quetiapine and now I’m steady. Also, stop weighing yourself daily. It’s torture. Weekly checks only. You got this!! 💪❤️
They don’t want you to lose weight because Big Pharma makes billions off diabetes meds. Metformin? It’s a gateway drug to insulin. Watch the FDA. They’re all in bed with the pharma giants. 🕵️♀️💊
This is why Indians are so healthy! We don't take these toxic Western pills!! My cousin took olanzapine and became fat and depressed, then he went to Ayurveda and now he runs 10km daily!! You need to stop the poison and go back to nature!!!
Lol metformin? That’s just a Band-Aid. The real problem? The government and pharma are forcing these meds on people to keep them docile. You think weight gain is the side effect? Nah. It’s the feature. You’re being chemically subdued. Wake up.
AMERICA IS WEAK. We let big pharma control our brains and then we whine about weight gain. In my day, you took your meds and you worked out. No excuses. Get off the couch. Stop blaming drugs. It’s laziness. Period.
i just started lurasidone and i swear i lost 5lbs in 2 weeks?? i think its bc i stopped eating cereal at 2am?? also i think my doc gave me the wrong dose but i dont wanna ask bc i dont wanna be that person??
The scientific evidence presented here is both comprehensive and clinically significant. It is imperative that patients engage in a multidisciplinary approach involving psychiatrists, dietitians, and behavioral therapists. Metformin, in particular, has demonstrated statistically significant efficacy in multiple randomized controlled trials. Consistency in monitoring metabolic parameters remains the cornerstone of long-term management.
Tim H, you’re not alone. I did the same. Cereal at 2am is my emotional support snack. But now I keep chia pudding in the fridge. Still sweet, but it doesn’t make me feel like trash. You’re doing better than you think.