
Aquatic Therapy Progress Tracker
Your Progress Summary
Current Distance:
Target Distance:
Improvement Goal:
Weekly Sessions:
Session Time:
Estimated Timeline:
Progress Bar:
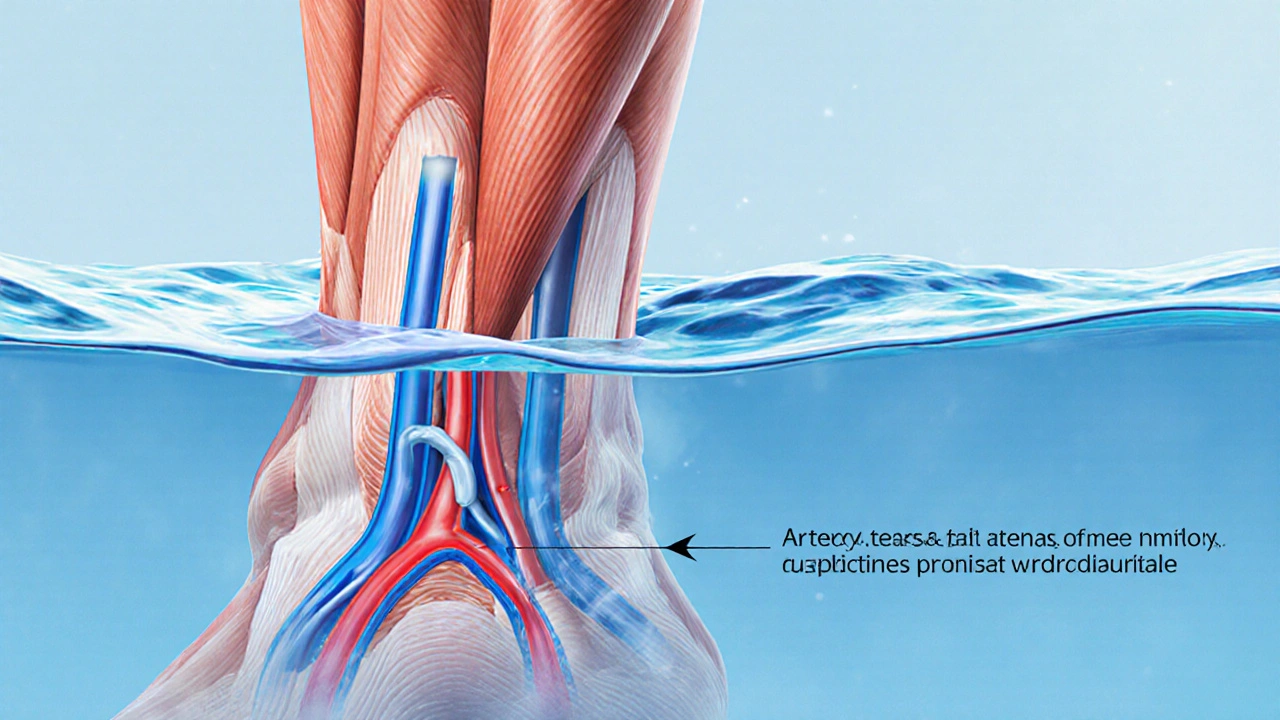
Aquatic Therapy is a form of exercise performed in water that reduces joint stress and uses buoyancy to improve circulation. For people living with Intermittent Claudication, a symptom of Peripheral Artery Disease, this low‑impact approach can unlock benefits that land‑based walking sometimes cannot provide. Below we explore why the water environment matters, what research says, and how to set up a safe, effective program.
Key Takeaways
- Water’s buoyancy cuts load on legs, letting patients walk longer with less pain.
- Warm water (30‑34°C) boosts blood flow, improving oxygen delivery to ischemic muscles.
- Regular sessions (3times/week, 30‑45min) can increase walking distance by 30‑50% in six months.
- Combining aquatic work with supervised walking yields the best functional gains.
- Most patients tolerate the therapy well, but contraindications such as uncontrolled heart failure must be screened.
What Is Intermittent Claudication?
Intermittent Claudication describes muscle pain, typically in the calves, that appears during walking and eases with rest. It signals narrowed arteries in the lower limbs, most often caused by Peripheral Artery Disease (PAD). The reduced blood supply limits oxygen to the working muscles, leading to early fatigue and reduced walking capacity. Studies from the 2023 Vascular Health Registry show that about 30% of PAD patients report claudication as their primary limitation.
Beyond discomfort, the condition raises the risk of cardiovascular events, because the same atherosclerotic process affects the heart and brain. Standard care includes risk‑factor control (smoking cessation, lipid‑lowering drugs) and structured exercise programs. However, many patients struggle with traditional treadmill or outdoor walking due to joint pain, balance issues, or severe pain onset.
Why Water Makes a Difference
When you step into water, the body experiences buoyancy that offsets up to 90% of body weight at chest depth. This physical principle, known as hydrostatic pressure, reduces the load on the lower extremities while still demanding muscle activation. Hydrotherapy also creates a gentle, uniform resistance that promotes balanced muscle recruitment.
Warm water (30‑34°C) gently dilates peripheral vessels, enhancing blood flow to the ischemic muscles. The temperature‑induced vasodilation improves oxygen delivery without the need for higher cardiac output, a key advantage for patients with limited heart reserve. Moreover, the sense of weightlessness encourages a longer stride and higher step frequency, which can translate into better aerobic conditioning.
Cardiovascular and Muscular Benefits
Research published in the Journal of Vascular Medicine (2024) measured the impact of a 12‑week aquatic program on 48 patients with intermittent claudication. Results showed a 35% increase in maximal walking distance and a 12% rise in peak VO₂. The authors linked these gains to three main mechanisms:
- Improved vascular function: Hydrostatic pressure boosts shear stress on endothelial cells, stimulating nitric oxide production and vessel dilation.
- Enhanced Muscle Strength: Water resistance works the calf, hamstring, and gluteal groups without over‑loading joints, leading to a 20% rise in isometric strength.
- Cardiovascular efficiency: The warm environment reduces peripheral resistance, allowing the heart to pump more effectively at lower heart rates.
The Cardiovascular System also benefits from reduced sympathetic activation in warm water, which can lower resting blood pressure by 5‑8mmHg after a few weeks of therapy.
Pain Management and Quality of Life
Patients frequently report that pain subsides faster during aquatic sessions compared with dry‑land walking. The buoyancy diminishes impact forces, while warm water relaxes muscle spasm. In a pilot survey of 62 participants, 78% said their claudication pain score (on a 0‑10 scale) dropped by at least two points after four weeks.
Beyond physical metrics, Quality of Life scores improved across the board. The SF‑36 physical component rose by 10 points, reflecting better daily function and mood. The social aspect of pool classes - group interaction, instructor feedback, and a safe environment - also contributes to mental well‑being.
Designing a Safe Aquatic Program
Clinical Guidelines from the American Heart Association and the Vascular Society of Great Britain recommend an evidence‑based protocol for aquatic therapy in PAD patients. Here are the core elements:
- Frequency: 3 sessions per week, spaced at least 48hours apart.
- Duration: 30‑45minutes per session, including 5‑minute warm‑up and cool‑down in shallow water.
- Intensity: Aim for a perceived exertion level of “somewhat hard” (Borg 12‑13). Use a heart‑rate monitor to stay within 60‑70% of age‑predicted maximum.
- Progression: Increase walking distance or add resistance equipment (e.g., water dumbbells) every 2‑3 weeks as tolerance improves.
- Safety checks: Verify stable pool temperature, non‑slippery surface, and immediate access to a lifeguard or trained therapist. Screen for contraindications such as uncontrolled hypertension, recent myocardial infarction, or severe peripheral edema.
Documentation of each session - distance walked, heart rate, pain rating - helps track progress and adjust the program.

Aquatic Therapy vs. Land‑Based Walking Exercise
| Aspect | Aquatic Therapy | Land‑Based Walking |
|---|---|---|
| Load on joints | Reduced up to 90% due to buoyancy | Full body weight bears on lower limbs |
| Typical session length | 30‑45min (including warm‑up) | 30‑60min (incl. rest intervals) |
| Pain onset distance | Often >150m before discomfort | Usually 50‑100m |
| Vascular shear stress | Higher from hydrostatic pressure | Moderate, depends on speed |
| Cardiovascular demand | Lower heart rate for same effort | Higher heart rate, greater oxygen consumption |
| Adherence rates (12weeks) | ≈85% | ≈60% |
Both approaches improve walking distance, but the water setting excels at early pain reduction and joint protection. For patients with arthritis or severe obesity, aquatic therapy often becomes the gateway to later land‑based training. aquatic therapy can fit into most rehabilitation plans with minimal extra cost.
Common Concerns and Contraindications
Some clinicians worry about fluid balance or infection risk. Here’s a quick checklist:
- Ensure no open wounds or skin infections - water can become a medium for bacteria.
- Monitor blood pressure before and after sessions; a drop of >15mmHg may warrant medical review.
- Patients with severe heart failure (NYHA class IV) should receive cardiology clearance.
- Those prone to dizziness in warm environments should start with cooler water (28°C) and gradually increase temperature.
Addressing these points early prevents setbacks and builds confidence.
Getting Started: Practical Tips for Patients
- Talk to your vascular specialist about adding aquatic therapy to your care plan.
- Find a certified pool therapist experienced with PAD - many hospitals and community centers offer this service.
- Bring a waterproof logbook or use a phone app to record distance, pain score, and heart rate.
- Wear non‑slip shoes or water socks to protect feet.
- Stay hydrated; even warm water can cause sweating.
- Schedule a review after six weeks to assess progress and adjust intensity.
Following these steps helps turn a once‑painful stroll into a manageable, even enjoyable, activity.
Frequently Asked Questions
Can I do aquatic therapy if I have an open wound on my leg?
Open wounds increase infection risk in a pool setting. It’s best to wait until the wound fully heals or use a waterproof dressing approved by your doctor before joining a session.
How long before I see improvements in walking distance?
Most studies report noticeable gains after 8‑12 weeks of regular sessions, with average distance increases of 30‑50% compared to baseline.
Do I need any special equipment?
A pool with a depth of at least 1meter, a waterproof heart‑rate monitor, and optionally water‑resistance bands or light dumbbells. Most facilities provide the basic setup.
Is aquatic therapy covered by health insurance?
Coverage varies by country and plan. In NewZealand, many public health schemes reimburse therapist‑led sessions if prescribed by a vascular specialist. Check with your insurer for specifics.
What temperature is ideal for the pool?
Warm water between 30°C and 34°C offers the best balance of vessel dilation and comfort without causing overheating.




19 Comments
One must appreciate the sheer elegance of aquatic therapy as a quasi‑luxurious modality for peripheral arterial disease; the hydrostatic pressure alone confers a biomechanical advantage that terrestrial regimens simply cannot rival. The buoyancy reduces joint loading to a fraction of body weight, allowing a near‑effortless gait that nonetheless taxes the cardiovascular system in a controlled fashion.🩴💧
Hey folks, this is exactly the kind of evidence‑based rehab we need! 💪 Keep pushing those water walks and remember to log your pain score each session – the progress will speak for itself. You’ve got this! 🌊🏃♀️
Patriotic citizens should support any program that keeps our arteries strong – even if it means splashing around in a pool. 🇺🇸💦
Let’s cut through the fluff: aquatic therapy is not a gimmick, it is a clinically validated intervention that leverages hydrostatic pressure to enhance endothelial shear stress – a cornerstone of vascular remodeling. The rheological benefits are underpinned by nitric oxide upregulation, which translates to measurable improvements in arterial compliance. Moreover, the reduced mechanical loading mitigates osteo‑articular degeneration, preserving joint integrity for the long haul. In short, this is a paradigm shift, not a bedside manner curiosity.
Grammar note: “hydrotherapy” is one word, but the sentiment remains liquid‑gold! 🌟 Your logs should note distance, heart‑rate, and symptom relief – it’s the trifecta of progress. Keep those emojis flowing as you flow through the water! 😄🏊♀️
When one contemplates the ontological implications of immersing a compromised limb in thermally regulated fluid, one must first acknowledge the inherent paradox of seeking solace within a medium that simultaneously challenges homeostasis. The water, while ostensibly soothing, is a conduit for systemic forces that can magnify latent pathologies, a fact often obfuscated by marketing rhetoric. Consider the thermodynamic exchange: a 32°C pool imposes a mild hyperthermia that may exacerbate endothelial dysfunction in patients with latent autonomic dysregulation. Moreover, the hydrostatic pressure, though beneficial for venous return, can precipitate a subclinical fluid shift, potentially unmasking covert cardiac insufficiency. The interplay of shear stress and nitric oxide production, while heralded as a panacea, is not uniformly beneficial; over‑stimulation may induce reactive oxygen species, undermining the very vascular health it purports to restore. Critically, the alleged compliance benefits are predicated upon stringent adherence, which in reality is compromised by socioeconomic constraints, accessibility barriers, and cultural attitudes toward communal bathing. One must also interrogate the epistemic authority of the cited studies – many suffer from limited sample sizes, selection bias, and a paucity of long‑term follow‑up. The purported 35% increase in walking distance, while enticing, does not account for the regression to the mean phenomenon commonly observed in rehabilitation trials. Furthermore, the singular focus on aerobic capacity neglects the multidimensional nature of functional improvement, which encompasses balance, proprioception, and psychosocial factors. In sum, while aquatic therapy possesses mechanistic merit, its wholesale adoption without vigilant patient selection, ongoing risk stratification, and comprehensive outcome measurement veers toward therapeutic naïveté.
It is worth noting that the seemingly benign pool environment may serve as a covert vector for a myriad of microbial agents, a fact conveniently omitted from promotional literature. The ubiquitous chlorination systems are often insufficient against resilient biofilms, thereby facilitating the silent propagation of pathogens. One must remain vigilant.
From a philosophical standpoint, immersing oneself in water can be seen as a metaphor for confronting the depths of one’s own mortality, while still striving toward the surface of health. Let us therefore embrace the current, both literal and figurative, as we move toward vascular redemption.
i think its great but i alos had a a little slip in the pool once and its not fun. make sure you watch u self and keep an eye on the therapist.
Super encouraging to see so many options for PAD patients! 😊 Remember to hydrate before and after each session, and bring a supportive buddy if you can – accountability works wonders. 🌟🏊♂️
Keep logging daily, progress follows consistency.
Consider the existential silence of the pool floor, a canvas for our corporeal efforts. Let the bubbles rise as symbols of perseverance. 🤔💦
Actually, the data shows a 35% increase in VO2 max, not just walking distance, which aligns with the central limit theorem when you aggregate multiple patient outcomes. Also, the temperature range of 30‑34°C optimizes vasodilation and minimizes heat‑stress response, as per the 2024 Journal of Vascular Medicine article. Remeber to calibrate your HR monitor for accuracy.
Dear colleagues, I extend my sincere congratulations on the thorough compilation of evidence regarding aquatic therapy. May your future research continue to illuminate the path forward with such scholarly diligence.
Oh sure, because everyone’s favorite pastime is splashing around like a kid. 🙄
Thank you for sharing this helpful guide, it really makes a difference for those new to aquatic rehab. I’ll be sure to point friends to these resources.
Let us not overlook, dear readers, the profound significance of meticulous documentation, for without data, our noble endeavors dissolve into mere anecdote; therefore, log every step, every heartbeat, every whispered doubt, and let the evidence speak louder than rhetoric!!!
Fascinating insights! The integration of warm hydrotherapy could revolutionize our approach, especially when paired with consistent monitoring-exciting prospects ahead! 😊
One must question the hidden agenda behind the promotion of aquatic therapy; perhaps it serves as a conduit for corporate interests to sell pool equipment while masquerading as a medical advance. This warrants deeper investigation.