When you’re prescribed betamethasone, it’s usually because other treatments haven’t worked. Maybe you have severe eczema, an autoimmune flare-up, or a respiratory condition that’s not responding. Betamethasone is powerful - it cuts inflammation fast. But that power comes with risks. Side effects aren’t rare. They’re common. And if you don’t know how to handle them, you could end up worse off than when you started.
What betamethasone actually does
Betamethasone is a synthetic corticosteroid. It mimics cortisol, your body’s natural stress hormone. But it’s 25 to 30 times stronger. That’s why it works so well for skin rashes, asthma attacks, or joint swelling. It shuts down immune signals that cause pain and redness. But it doesn’t just target the problem area. It floods your whole system. That’s where side effects come from.
It comes in creams, injections, tablets, and even nasal sprays. Each form has different risks. A cream on your face might cause thinning skin. A shot in your knee might raise your blood sugar. Pills taken for weeks? That’s when things get serious.
Common side effects you can’t ignore
Not all side effects are scary. Some are just annoying. But if you treat them like normal, they can turn into real problems.
- Skin thinning - Especially with long-term cream use. Your skin might look shiny, bruise easily, or develop stretch marks. This isn’t just cosmetic. It increases infection risk.
- Acne or facial hair - Even women who never had acne before might get it. It’s not just stress or diet. It’s the steroid changing your hormone balance.
- Increased appetite and weight gain - You’re not lazy. Betamethasone makes your body hold onto fat, especially around your belly and face. This is called "moon face" - a telltale sign of steroid use.
- Insomnia and mood swings - You might feel wired at night, then crash during the day. Some people get anxious, irritable, or even depressed. This isn’t "just in your head." It’s the drug affecting brain chemistry.
- High blood sugar - Even if you’ve never had diabetes, betamethasone can spike your glucose. If you’re overweight or have a family history, this is a red flag.
These aren’t "maybe" risks. A 2023 study in the Journal of Dermatology found that over 60% of people using topical betamethasone daily for more than 4 weeks developed some form of skin damage. And 40% of oral users saw blood sugar rise above normal levels within two weeks.
How to prevent side effects before they start
Prevention isn’t about avoiding the drug. It’s about using it smarter.
- Use the lowest dose possible - Your doctor might start you on a strong dose to get things under control. But after a few days, ask if you can drop down. Many people stay on high doses too long because they forget to check in.
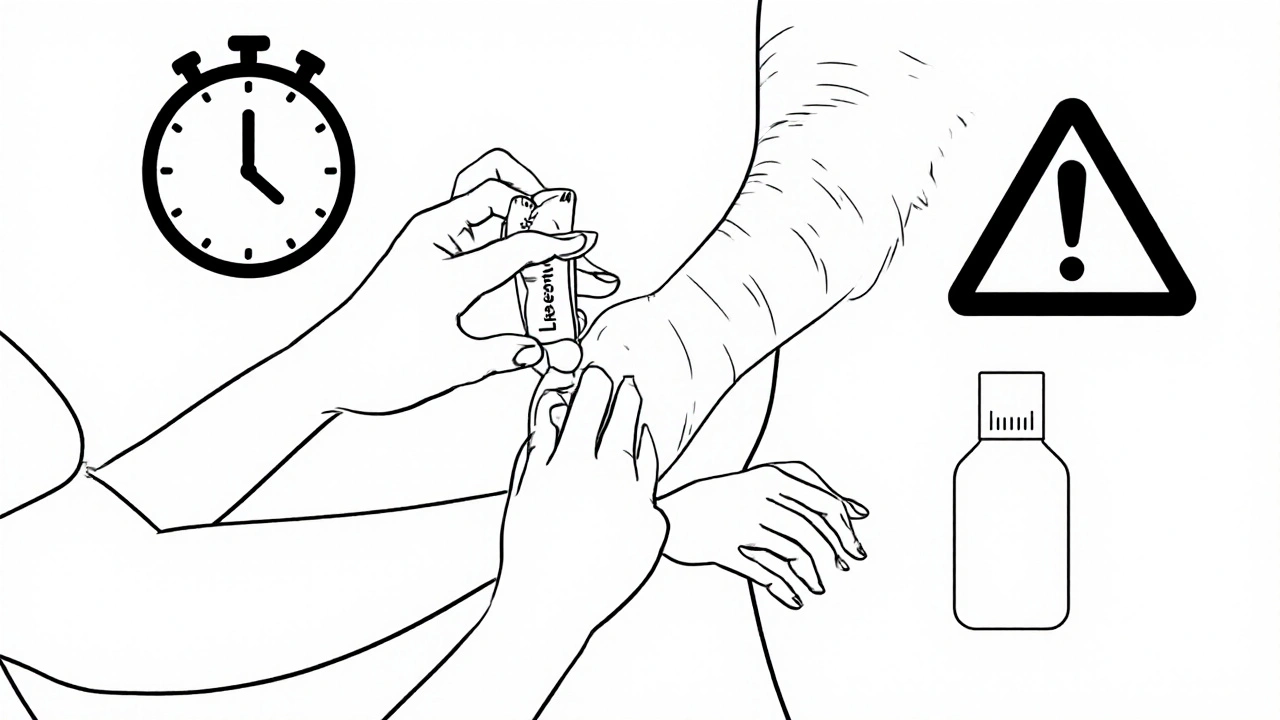
- Limit duration - Topical betamethasone shouldn’t be used on the same area for more than 2 weeks straight. For oral use, most courses last 5 to 10 days. Longer than that? You need a new plan.
- Avoid sensitive areas - Never use strong creams on your face, armpits, groin, or eyelids unless your doctor specifically says so. These areas absorb steroids faster. The skin there is thinner. The damage happens quicker.
- Don’t combine with other steroids - If you’re using a nasal spray, inhaler, or eye drops with steroids, you’re adding to the total load. Tell your doctor about every product you’re using.
- Take oral doses in the morning - Your body naturally releases cortisol early in the day. Taking betamethasone then mimics that rhythm. It lowers the chance of sleep problems and reduces adrenal suppression.
Managing side effects while you’re still on the drug
You’re already on betamethasone. You can’t just stop. But you can reduce the damage.
- For skin thinning - Use a fragrance-free moisturizer twice a day. Look for ceramides or hyaluronic acid. They help rebuild your skin barrier. Avoid scrubs, alcohol-based toners, or hot showers. These strip what’s left.
- For weight gain and appetite - Eat protein and fiber first at meals. They fill you up faster. Avoid sugary snacks and refined carbs. They spike insulin, which makes fat storage worse. A 2024 trial showed patients who followed a high-protein, low-glycemic diet gained 40% less weight on steroids than those who didn’t.
- For high blood sugar - Check your glucose if you can. Even a simple home monitor helps. Cut back on juice, white bread, and pasta. Walk for 20 minutes after meals. Movement helps your body use sugar better.
- For mood changes - Talk to someone. Don’t bottle it up. Exercise helps - even a daily walk. If you feel hopeless or have thoughts of self-harm, call your doctor immediately. Steroid-induced depression is real and treatable.
- For insomnia - No screens after 8 p.m. Keep your room cool. Try magnesium glycinate before bed. It’s gentler than melatonin and helps with steroid-related nerve overactivity.
What to do when side effects get worse
Some side effects need urgent attention.
- Swelling in your ankles, feet, or hands - This could mean fluid retention from salt and water buildup. It’s a sign your kidneys are struggling. Call your doctor. You might need a diuretic.
- Blurred vision or eye pain - Betamethasone can increase eye pressure. Untreated, this leads to glaucoma. Get your eyes checked within a week if this happens.
- Feeling dizzy, nauseous, or weak - These could be signs your adrenal glands have shut down. Your body stopped making its own cortisol because the drug took over. Suddenly stopping betamethasone now could cause adrenal crisis - a life-threatening drop in blood pressure. Never quit cold turkey.
How to safely stop betamethasone
Stopping is just as important as starting. Tapering isn’t optional. It’s medical necessity.
For oral betamethasone, your doctor will slowly lower your dose over days or weeks. For example, if you were on 1 mg daily, you might drop to 0.75 mg for 5 days, then 0.5 mg, then 0.25 mg, then stop. This gives your adrenal glands time to wake up.
For topical use, switch to a weaker steroid for a week before stopping completely. Or use the cream every other day instead of daily. This prevents rebound inflammation - where your original condition comes back worse than before.
Never stop based on how you feel. If your rash is gone, that doesn’t mean your body is ready. You need a plan.
What to do after you stop
Once you’re off betamethasone, your body is still recovering.
- Watch for rebound symptoms - Your original condition might return. That doesn’t mean you failed. It means your body needs support. Talk to your doctor about alternatives like calcineurin inhibitors (tacrolimus, pimecrolimus) for skin, or leukotriene inhibitors for asthma.
- Rebuild your skin - Use gentle cleansers. Avoid exfoliants for at least 3 months. Consider a dermatologist-recommended barrier repair cream. It takes time, but your skin will heal.
- Monitor your weight and blood sugar - These can stay elevated for weeks after stopping. Keep eating well and moving. Most people return to normal within 6 to 8 weeks.
- Get your adrenal function checked - If you were on oral betamethasone for more than 3 weeks, ask for an ACTH stimulation test. It checks if your adrenal glands are working again.
When to call your doctor
You don’t need to wait for a crisis. Call if:
- Your skin breaks open or gets infected
- You’re urinating more than usual or feeling thirsty all the time
- You have chest pain, shortness of breath, or irregular heartbeat
- You feel unusually tired, cold, or confused
- You’re taking betamethasone and get sick with fever, flu, or an injury
These aren’t "maybe" signs. They’re red flags. Betamethasone suppresses your immune system. A small infection can become dangerous fast.
Alternatives to consider
There are other options. Some work slower. But they’re safer long-term.
- For eczema - Crisaborole (Eucrisa) or topical calcineurin inhibitors (Protopic, Elidel) don’t thin skin. They’re safe for kids and long-term use.
- For asthma - Inhaled corticosteroids like fluticasone are targeted. They don’t flood your body like pills.
- For autoimmune conditions - DMARDs like methotrexate or biologics like adalimumab control inflammation without the steroid side effects.
Ask your doctor: "Is there a safer option I can try after this course?" Most will have one.
Can betamethasone cause permanent damage?
Yes, if used improperly. Long-term use of high-dose oral betamethasone can lead to osteoporosis, cataracts, or adrenal insufficiency that lasts months or years. Skin thinning from creams can be permanent in some cases, especially if used on delicate areas. But most side effects reverse if you stop correctly and give your body time to recover.
Is betamethasone safe for children?
Topical betamethasone can be used in children, but only under strict supervision. It’s not recommended for infants under 3 months. For older kids, use the weakest strength possible, limit to 1 week, and avoid the face and diaper area. Long-term use can stunt growth. Always check with a pediatric dermatologist or allergist.
Can I drink alcohol while taking betamethasone?
It’s not recommended. Alcohol increases stomach irritation and raises your risk of ulcers - a known side effect of steroids. It also worsens liver stress and can make mood swings worse. If you’re on oral betamethasone, skip the alcohol until you’re completely off it.
How long do side effects last after stopping?
It depends. Skin changes like thinning or stretch marks may take months to improve. Weight gain often reverses in 4 to 8 weeks with diet and exercise. Blood sugar usually returns to normal within 2 weeks. Adrenal recovery can take 3 to 12 months, especially after long-term use. Don’t rush back to normal life - give your body space to heal.
Are there natural ways to reduce betamethasone side effects?
There’s no natural substitute for betamethasone, but you can support your body. Eat calcium-rich foods (dairy, leafy greens) and vitamin D to protect bones. Take magnesium to help with sleep and muscle cramps. Stay hydrated. Avoid processed sugar. Exercise gently. These won’t replace the drug, but they help your body handle it better.
Final thought: Power needs responsibility
Betamethasone isn’t evil. It’s a tool. Like a chainsaw - it can save your life or hurt you badly. The difference is how you use it. Follow your doctor’s instructions. Ask questions. Don’t assume side effects are normal. Track how you feel. And never, ever stop without a plan. Your body will thank you.



12 Comments
Just finished my 3-week course and wow-my skin feels like tissue paper now. But honestly? Worth it. The rash was killing me. Just started using ceramide cream twice daily and it’s already less scary. Stay strong, everyone.
Hey, I’m a nurse and I’ve seen this so many times. People panic when they get moon face or acne and quit cold turkey-big mistake. Tapering is NON-NEGOTIABLE. I had a patient last month who went from 1mg to zero in 2 days… ended up in ER with adrenal crash. Please, if you’re on this, talk to your doc before making changes. You’re not weak for needing help-you’re smart for asking.
While the article presents a clinically sound overview, one must consider the epistemological limitations of patient-reported outcomes in the context of glucocorticoid pharmacodynamics. The cited 2023 study, while informative, employs a convenience sample with limited demographic diversity. Furthermore, the assertion that "side effects are common" lacks a quantified baseline against which to measure prevalence relative to placebo or alternative therapies. A more rigorous meta-analysis would enhance the validity of these claims.
Man, I used this cream for my eczema last year. Thought it was magic till my face started peeling. Didn’t know you’re not supposed to use it on your face. My bad. Now I use that Eucrisa stuff like the article said. No more scary skin. Just say no to strong steroids on your face, folks.
So let me get this straight… we’re being told to use a chemical that turns your body into a walking side effect catalog… but the real villain is… not following the instructions? Wow. What a revelation. Next they’ll tell us that breathing oxygen too much causes lung damage. Oh wait-it does. And we’re still alive. Maybe the real issue is that Big Pharma makes these drugs so damn effective that we forget they’re basically biological arson. Taper? Sure. But why not just… not start it in the first place? Just sayin’.
I’m so glad someone finally wrote this. I’ve been telling my friends for months: don’t ignore the acne. Don’t brush off the weight gain. Don’t think insomnia is "just stress." I was on this for 6 weeks and I thought I was going crazy. Turns out, it was the drug. Now I’m off, and my sleep’s back. Thank you for the magnesium tip. I’m trying it tonight. Seriously, this is life-changing info.
They never tell you the truth. Betamethasone? It’s not just a drug-it’s a gateway to the pharmaceutical surveillance state. Your adrenal glands? They’re being reprogrammed. The "tapering"? A placebo ritual to make you feel safe while they keep you hooked. And don’t get me started on the "alternatives"-calcineurin inhibitors? They’re just the next step in the slow-kill protocol. Wake up. The system doesn’t want you healthy. It wants you dependent. Check the patents. Check the funding. This isn’t medicine. It’s control.
I’m from India and we use betamethasone cream all the time here-often without prescription. My aunt used it for years for her psoriasis. Skin got thin, yes. But she also got diabetic. Now she’s on insulin. This article is spot on. Please, if you’re using it, get your sugar checked. And don’t use it on kids unless a doctor says so. I’ve seen too many kids with stunted growth because of this. Good advice here.
Just wanted to say thank you for writing this. I’ve been helping my sister through her steroid treatment and honestly? I was terrified. This guide gave me so much clarity. I printed it out and we’re using it as our checklist. Low dose, morning pills, no alcohol, moisturizer every night. Small steps. Big difference. You’re not just giving info-you’re giving hope.
OMG I just realized I’ve been using betamethasone on my inner thighs for 18 months because "it’s the only thing that works"-and now I have stretch marks that look like lightning bolts. I’m not mad, I’m just… wow. Also, why is everyone so chill about this? Like, this is basically chemical warfare on your body and we’re treating it like a spa treatment? 🤯 Also, "calcineurin inhibitors"? Sounds like a sci-fi villain. I’m switching to witch hazel and vibes now. ✨
Thanks for this. I didn’t know about the morning dose thing. I was taking mine at night and wondering why I couldn’t sleep. Now I’m switching to morning. Also, the part about not combining with other steroids? I had that nasal spray and didn’t realize it counted. Oops. I’m gonna talk to my doctor this week. You’re right-this stuff is powerful. Gotta respect it.
Bro, this is gold! 🙏 I’ve been on this for 5 weeks and my face is puffy like a chipmunk 😅 But now I’m eating protein first, walking after meals, and using that ceramide cream. My skin is slowly coming back. Also, magnesium glycinate? I bought it! 🤘 Stay safe, stay smart, and don’t quit cold turkey-your adrenals will thank you later! 💪