
Every year, millions of Americans grab an OTC medicine off the shelf without thinking twice. Headache? Grab a pill. Cold symptoms? Pick up a bottle. But here’s the problem: OTC drug facts labels are designed to be clear - yet most people skip them. And that’s where mistakes happen.
You might not realize it, but taking two different cold medicines at once could mean you’re accidentally doubling your dose of acetaminophen. That’s dangerous. In fact, accidental acetaminophen overdoses send over 50,000 people to the ER each year. The good news? You don’t need to be a pharmacist to read these labels correctly. You just need to know where to look - and what to ignore.
What’s on the OTC Drug Facts Label?
The U.S. Food and Drug Administration (FDA) made these labels mandatory in 2017. Before that, every brand had its own layout - confusing, inconsistent, and often misleading. Now, every OTC medicine sold in the U.S. must follow the same format. That means if you learn how to read one label, you can read them all.
There are seven sections you need to know:
- Active Ingredients
- Purpose
- Uses
- Warnings
- Directions
- Other Information
- Inactive Ingredients
They’re always in this exact order. No exceptions. That’s by design - so you don’t have to hunt for info.
Active Ingredients: The Most Important Part
This is where you start - and where most people stop. But this section holds the key to avoiding dangerous mistakes.
Look for the chemical name, not the brand name. Tylenol? That’s just a brand. The active ingredient is acetaminophen. Advil? That’s ibuprofen. DayQuil? It contains acetaminophen, dextromethorphan, and phenylephrine.
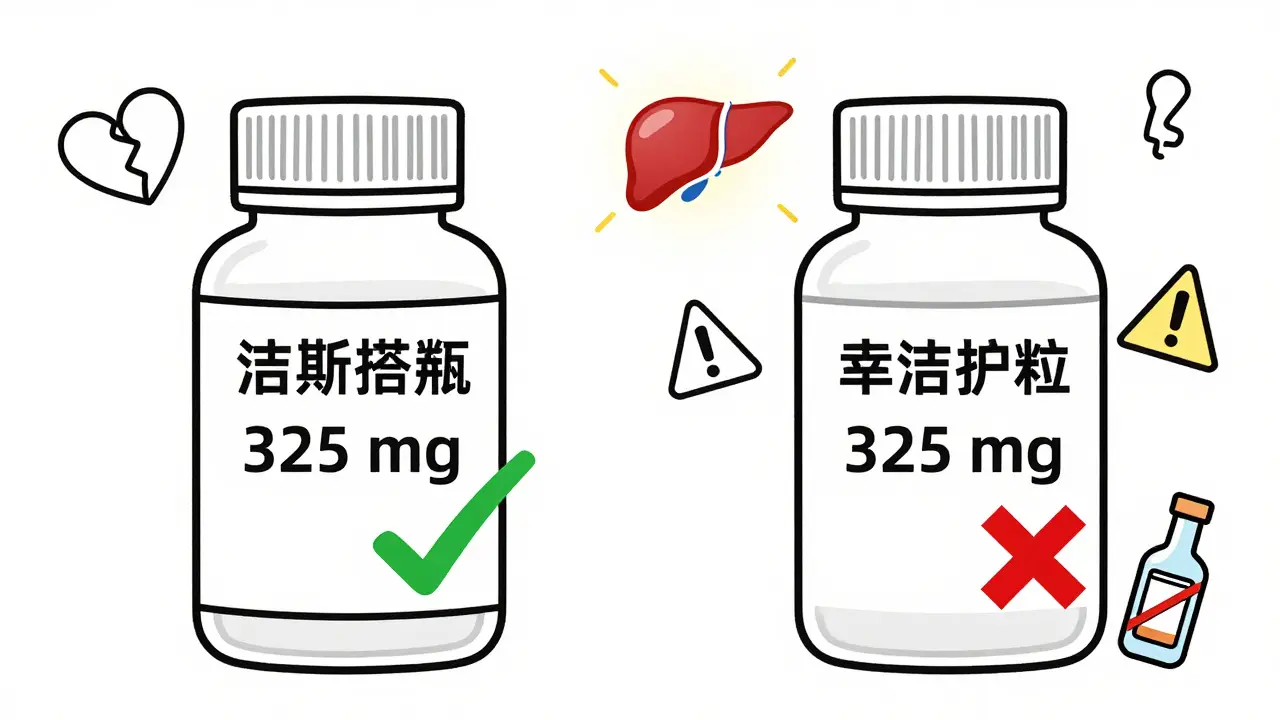
Each ingredient is listed with its amount per dose. For example: “Acetaminophen 325 mg” means each tablet or capsule has 325 milligrams. Liquid forms say it per volume - like “160 mg per 5 mL”.
Why does this matter? Because if you’re taking two products that both contain acetaminophen - say, a cold medicine and a pain reliever - you could easily hit the 4,000 mg daily limit without realizing it. That’s when liver damage becomes a real risk. In 2023, the FDA reported that 67% of people who checked the active ingredients avoided accidental overdoses. The rest? They didn’t.
Purpose: What Does It Do?
Right under the active ingredients, you’ll see “Purpose.” This tells you what each ingredient is supposed to do. For example:
- Pain reliever / fever reducer
- Cough suppressant
- Nasal decongestant
- Antihistamine
This helps you match the medicine to your symptoms. If you only have a sore throat, you don’t need a medicine that also has a decongestant. That’s extra chemicals your body doesn’t need.
Also, watch out for multi-symptom products. They’re convenient - but they’re also the most likely to cause accidental overdoses. If you’re only treating one thing, choose a single-ingredient product.
Uses: What It’s Approved For
This section is short and strictly regulated. The FDA doesn’t allow vague claims like “supports immune health” or “boosts energy.” Instead, it lists exactly which symptoms the medicine can treat.
For example: “Temporarily relieves minor aches and pains due to headache, toothache, menstrual cramps, or the common cold.”
If your symptom isn’t listed here, don’t use the product for it. That’s not just ineffective - it’s risky. A 2023 study found that 72% of older adults used OTC medicines for symptoms not listed on the label - and nearly half ended up with side effects.
Warnings: Don’t Skip This
This is the section that saves lives. And yet, 41% of people skip it entirely, according to FDA consumer studies.
Here’s what to look for:
- Do not use if... - Allergies, existing conditions like liver disease, or pregnancy.
- Ask a doctor before use if... - You’re on blood thinners, have high blood pressure, or are over 60.
- Liver warning: - If the product contains acetaminophen, it will say: “Severe liver damage may occur if you take more than 4,000 mg in 24 hours.”
- Stomach bleeding warning: - For NSAIDs like ibuprofen or naproxen, it will warn about risk if you’re over 60, take blood thinners, or have a history of ulcers.
- Do not use with alcohol. - Especially with acetaminophen or sedating antihistamines.
Pharmacists say the warnings section is the single most important part of the label. In a 2023 survey of 1,200 pharmacists, 89% said it was the section that prevented the most adverse events.
Directions: Dose, Frequency, Duration
This is where people get tripped up - especially with liquids and children’s doses.
Look for:
- Who it’s for - “Adults and children 12 years and older”
- How much - “2 caplets” or “10 mL”
- How often - “Every 4 to 6 hours”
- How many in 24 hours - “Do not take more than 8 caplets in 24 hours”
- How long - “Do not use for more than 10 days unless directed by a doctor.”
Common mistakes:
- Confusing “5 mL” with the whole bottle. A 4-ounce bottle of Children’s Motrin holds 118 mL - that’s over 20 doses. Don’t assume the whole bottle is one dose.
- Thinking “extra strength” means you can take more. Extra strength just means more active ingredient per dose. The daily limit stays the same.
- Assuming “PM” means safer. Most nighttime cold medicines contain diphenhydramine (38 mg per dose) - a powerful antihistamine that causes drowsiness. It’s not meant for daily use.
For kids, always use the measuring tool that comes with the medicine. Kitchen spoons are not accurate. A teaspoon is 5 mL - but a soup spoon can be 10 mL or more.
Other Information: Storage and Extras
This section includes:
- Storage instructions - “Store between 68°F and 77°F.” Heat and moisture ruin medicine.
- Sodium content - “Each tablet contains 2 mg sodium.” Important for people on low-sodium diets.
- Expiration date - Always check this. Expired medicine doesn’t necessarily become toxic, but it loses effectiveness.
Don’t ignore this. If you keep medicine in the bathroom, it’s getting hot and moist. That’s not where it belongs.
Inactive Ingredients: Hidden Allergens
This is the section most people overlook - but it can be critical.
Inactive ingredients include fillers, dyes, and preservatives. They don’t treat your symptoms - but they can trigger allergies.
Look out for:
- FD&C Red No. 40 - a common dye that can cause reactions in sensitive people.
- Gluten - not always listed as “wheat,” but sometimes as “modified starch” or “dextrin.”
- Lactose - common in tablets. People with lactose intolerance may have stomach upset.
- Alcohol - sometimes used as a solvent. Not always obvious.
If you have food allergies or sensitivities, this section matters. A 2024 study found that 12% of people with known allergies had reactions to OTC medicines because they didn’t check inactive ingredients.

How to Use This Like a Pro: The 5-Point Check
Pharmacists at CVS Health developed a simple method called the “5-Point Check.” It takes about 50 seconds - but it cuts your risk of error by two-thirds.
- Identify active ingredients - Write them down if you need to. Don’t trust your memory.
- Verify uses match your symptoms - If it doesn’t list what you have, don’t take it.
- Read all warnings - Especially liver, stomach, and interaction warnings.
- Check directions for age and weight - Kids, seniors, and people with chronic conditions need special care.
- Review inactive ingredients - For allergies or dietary needs.
Use this every time - even if it’s the same medicine you’ve taken before. Labels change. So do your health conditions.
What’s Changing Soon?
The FDA is making updates. Starting in 2025, new labels will feature:
- Larger font for active ingredient concentrations
- Color-coded sections
- Simple icons for warnings (like a liver symbol for acetaminophen)
Some brands are already adding QR codes that link to video explanations. You can scan them with your phone to hear a pharmacist explain the label in plain language.
These changes are coming because 41% of people still can’t find the maximum daily dose on current labels. The goal? Cut emergency visits by another 25% by 2027.
What to Do If You’re Still Confused
You don’t have to figure this out alone.
Pharmacists are trained to help with OTC medicine questions - and they’re usually free to ask. Walgreens reported a 40% increase in OTC consultations after launching their “Label Literacy” campaign in 2023.
There’s also a free FDA app called “Drug Label Decoder.” It lets you scan a barcode or type in a medicine name and shows you the label in plain text with explanations. Over 1.2 million people have downloaded it since August 2023.
And if you’re ever unsure - pause. Wait. Call your pharmacist. It’s better to wait five minutes than risk an overdose.
OTC medicines are powerful. They’re not candy. They’re not harmless. But when you know how to read the label, they’re also safe - and effective. You don’t need to be an expert. Just careful.
Can I take two OTC medicines at once if they’re for different symptoms?
Only if you check the active ingredients. Many cold, flu, and pain medicines contain the same ingredients - like acetaminophen or ibuprofen. Taking two products with the same active ingredient can lead to overdose. Always compare the active ingredients before combining medicines.
What’s the difference between “active” and “inactive” ingredients?
Active ingredients are the chemicals that treat your symptoms - like acetaminophen for pain or pseudoephedrine for congestion. Inactive ingredients are fillers, dyes, or preservatives that help the medicine hold its shape or taste better. They don’t treat anything - but they can cause allergic reactions in some people.
Is it safe to use expired OTC medicine?
Most expired OTC medicines are not dangerous, but they may not work as well. The FDA says potency can drop after expiration. For life-saving medications like epinephrine, never use expired. For pain relievers or antihistamines, if it’s only a few months past expiration and stored properly, it’s usually fine - but don’t rely on it for serious symptoms.
Why do some labels say “do not use” for people with high blood pressure?
Many cold medicines contain decongestants like phenylephrine or pseudoephedrine. These shrink blood vessels - including those in your nose. But they also raise your blood pressure. If you have uncontrolled high blood pressure, taking these can lead to stroke or heart attack. Always check the warnings if you have heart or blood pressure issues.
Can I give adult OTC medicine to my child if I reduce the dose?
No. Adult medicines are formulated for body weight and metabolism that children don’t have. Even a reduced dose can be dangerous. Always use a medicine made for children - it’s dosed by weight and has the right inactive ingredients. Never guess - use the label on the children’s product.
How do I know if a medicine contains acetaminophen if it’s not called Tylenol?
Look for the word “acetaminophen” on the active ingredients list. It’s the only official name. Brand names like Tylenol, Excedrin, NyQuil, and many cold medicines all contain it. If you see “APAP” on the label, that’s also acetaminophen - it’s the chemical abbreviation.
Next Steps: Make It a Habit
Start today. The next time you pick up an OTC medicine - whether it’s for a headache, a cough, or a fever - pause. Read the label. Use the 5-Point Check. Write down the active ingredients if you need to.
Teach your kids how to read them too. Older adults? Help them with the font size - use a magnifying glass or the FDA app. Your pharmacist isn’t just there for prescriptions - they’re your free, expert guide for everything on the shelf.
OTC medicines are meant to help you - not hurt you. But only if you know how to use them. You’ve got the power. Just don’t skip the label.


1 Comments
So let me get this straight... we need a PhD just to pick out a painkiller? 🤡
Next they'll make us pass a quiz before buying aspirin.