
When it comes to catching lung cancer early, low-dose CT screening isn’t just another test-it’s one of the few tools proven to save lives. But not everyone qualifies, and not every result means cancer. Understanding who should get screened and what the results actually mean can make all the difference.
Who Should Get Screened?
The guidelines have changed. In 2013, only people aged 55 to 80 with a 30-pack-year smoking history were eligible. Today, the standard has expanded. According to the U.S. Preventive Services Task Force (USPSTF), you qualify if you’re between 50 and 80 years old, have smoked at least 20 pack-years, and either still smoke or quit within the last 15 years.A pack-year is simple: one pack a day for one year equals one pack-year. Two packs a day for 10 years? That’s 20. Half a pack a day for 40 years? Also 20. It’s not about how hard you smoked-it’s about total exposure.
But here’s where things get tricky. The Centers for Medicare & Medicaid Services (CMS) still uses an older cutoff: age 50 to 77. That means if you’re 78 and eligible under USPSTF rules, you might not get coverage unless your insurance covers it. Meanwhile, the American Cancer Society and National Comprehensive Cancer Network (NCCN) have gone even further-removing the 15-year quit limit entirely. They argue that lung cancer risk stays high for decades after quitting. Data shows 34% of lung cancers occur in people who quit more than 15 years ago.
And it’s not just smoking. If you have a family history of lung cancer, were exposed to asbestos, radon, or diesel fumes, or have scarring in your lungs from past infections or diseases like pulmonary fibrosis, you might still benefit. The NCCN says these factors should be considered, even if you don’t meet the smoking criteria.
How Does Low-Dose CT Work?
Unlike a regular chest X-ray, which shows only the big picture, low-dose CT takes hundreds of thin slices of your lungs. It’s quick-less than 10 seconds. You lie on a table, hold your breath, and that’s it. No needles. No fasting. No prep.The radiation is tiny. A standard chest CT might give you 7 mSv. A low-dose CT? Around 0.8 to 1.5 mSv. That’s less than half the radiation you get from natural background sources in a year. Modern machines use advanced software to cut dose even further without losing detail. The American College of Radiology requires all accredited centers to stay under 1.5 mSv.
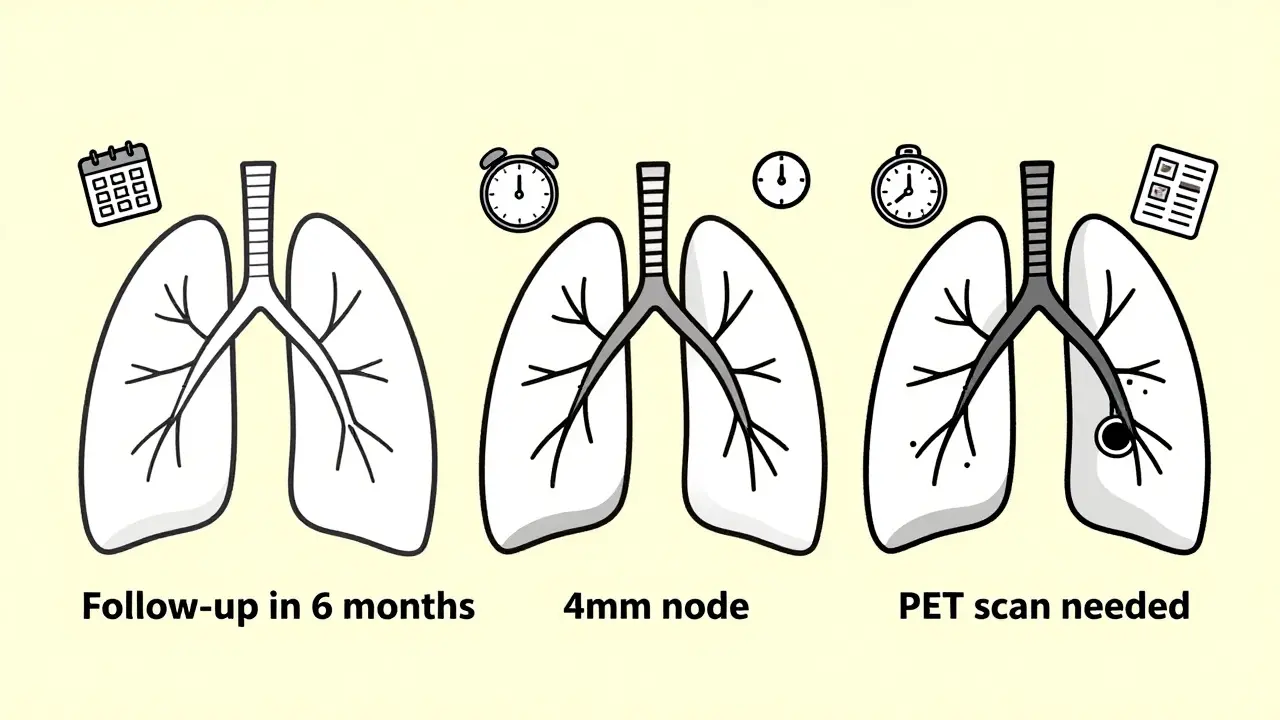
The images are reviewed by radiologists trained in lung screening. They look for nodules-small spots on the lungs. Most are harmless. But if a nodule is 4 mm or larger, it triggers further action. The goal isn’t to find cancer right away-it’s to catch it before it spreads.
What Do the Results Mean?
Most people get a clean bill of health. But about 20-25% of first-time screenings show something unusual. That doesn’t mean cancer. In fact, 96% of positive screens turn out to be benign.Here’s how it breaks down:
- 4-6 mm nodules: These are the most common. Doctors usually recommend a follow-up scan in 6 months. Less than 1% become cancerous in two years.
- 6-8 mm nodules: More concern. A repeat scan in 3-6 months is typical. Some centers use AI tools to measure growth more precisely.
- Over 8 mm: This usually leads to a PET scan or biopsy. The chance of cancer here jumps to 15-30%.
The National Lung Screening Trial found that LDCT detected three times more early-stage cancers than chest X-rays. And of those cancers found, 71% were Stage I-the most treatable stage. That’s huge. Stage I lung cancer has a 90% five-year survival rate if treated.
But false positives come with a cost. A 2023 study found that 42% of people experienced anxiety while waiting for follow-up tests. One patient in Ohio spent $450 and three months of stress before doctors confirmed her nodule was benign. That’s why shared decision-making is required before screening. You need to know what you’re signing up for.
What Happens If Something Is Found?
If a nodule grows or looks suspicious, you’ll be referred to a team that includes a pulmonologist, thoracic surgeon, and oncologist. The next step is often a high-resolution CT or PET scan. If cancer is confirmed, surgery is usually the first option.Most surgeries today are done with video-assisted thoracoscopic surgery (VATS)-tiny incisions, camera-guided, no cracked ribs. Hospital stays are down to 3 days on average, compared to over 5 years ago. Recovery is faster, pain is lower.
But not all cancers are caught early. Some grow fast. Others are hidden. That’s why annual screening matters. Skipping a year can mean missing the window.
Why Isn’t Everyone Getting Screened?
Despite the evidence, only about 23% of eligible Americans get screened. That’s not because people don’t care. It’s because of access.In rural areas, the average distance to a screening center is 32 miles. Many don’t have reliable transportation. Others don’t know they qualify. A CDC study found that Black Americans are 28% less likely to be screened than White Americans-even though they have higher lung cancer rates.
Medicaid expansion helped. States that expanded Medicaid saw screening rates 37% higher than those that didn’t. Insurance coverage matters. Medicare covers it 100% with no copay. Most private insurers follow suit. But if you’re uninsured or underinsured, it’s still a barrier.
And then there’s fear. The word “cancer” terrifies people. Some avoid screening because they’re scared of what they might find. Others don’t want to deal with the anxiety of follow-up tests-even if they’re almost always negative.

The Bigger Picture: Is It Worth It?
The numbers are clear. For every 1,000 people screened annually for 6.5 years, 15 lung cancer deaths are prevented. The radiation risk? About 1 extra cancer death per 1,000. That’s a net gain.Cost-wise, screening costs $2.8 billion a year if everyone eligible gets it. But it saves $6.3 billion in treatment, lost productivity, and early deaths. That’s a return of over $2 for every dollar spent.
And it’s getting smarter. AI tools now help radiologists spot nodules faster and more accurately. One FDA-approved system reduced reading time by 30% without missing a single cancer. Blood tests are coming too-tests that detect cancer DNA in the bloodstream. They’re not ready yet, but they’re close.
The real question isn’t whether LDCT works. It’s whether we’re doing enough to reach the people who need it most.
What’s Next?
In January 2024, CMS announced it’s reconsidering its rules. They’re looking at removing the 15-year quit limit and raising the upper age limit to 80. If they do, an extra 12,000 lives could be saved each year.Meanwhile, researchers are building better risk models. One called LYFS-CT uses age, smoking history, lung function, and family history to predict who benefits most. It could cut unnecessary scans by 27% while catching more cancers.
But until then, if you’re 50 or older, have smoked 20 pack-years or more, and still smoke or quit within the last 15 years-you should talk to your doctor. No one else will bring it up. You have to ask.
Do I need a referral to get a low-dose CT scan for lung screening?
Yes, you usually need a referral from a doctor. Medicare and most insurers require a shared decision-making visit before scheduling the scan. During this visit, your provider will review your risk factors, explain the benefits and risks, and answer your questions. This isn’t just a formality-it’s required for insurance coverage.
Is low-dose CT the same as a regular chest CT?
No. A regular chest CT uses higher radiation to get detailed images for diagnosing illness. A low-dose CT uses only about 10% of that radiation, just enough to detect nodules. It’s not meant to diagnose pneumonia or heart issues-it’s built for one thing: finding early lung cancer.
What if I quit smoking more than 15 years ago? Can I still get screened?
Under current Medicare rules, no. But the USPSTF and American Cancer Society say you might still benefit. Studies show lung cancer risk stays elevated for over 25 years after quitting. If you’re healthy and have other risk factors, talk to your doctor. Some private insurers and clinics are starting to screen people who quit longer ago.
How often should I get screened?
Annually. The evidence shows yearly screening reduces lung cancer deaths the most. Skipping even one year increases your risk of missing a growing nodule. If you’re still smoking or have a history of heavy smoking, don’t stop. The benefit drops if you don’t keep up with annual scans.
Are there any risks to low-dose CT screening?
Yes. The biggest risk is a false positive-finding something that looks like cancer but isn’t. This can lead to more scans, biopsies, and anxiety. There’s also a tiny radiation risk, but it’s far smaller than the benefit. For every 1,000 people screened, about 15 lung cancer deaths are prevented, and only 1 extra cancer might be caused by radiation. The trade-off is strongly in your favor.



