
When you’ve tried every gentle cleanser and still see a flare‑up of Rosacea a chronic inflammatory skin disorder that causes facial redness, visible blood vessels, and occasional bumps, the question “Can Hydrocortisone a low‑potency topical corticosteroid that reduces swelling and itching help calm that fire?” pops up for many people.
What is Hydrocortisone and How Does It Work?
Corticosteroid a class of steroid hormones that mimic the natural hormone cortisol are the backbone of many skin creams. Hydrocortisone belongs to the low‑strength end of that family, usually 0.5 % to 2.5 % in over‑the‑counter gels and ointments. The drug binds to glucocorticoid receptors in skin cells, telling them to dial down Inflammation the body’s response that causes redness, heat, and swelling. By interrupting the cascade of inflammatory chemicals, the visible “flare” of rosacea can shrink within a few days.
Typical Prescription Details for Rosacea
Doctors rarely hand out a prescription for “hydrocortisone for rosacea” without a clear plan. The usual recommendation is a short course-often 1 % cream applied once or twice daily for no more than two weeks. The goal is to knock down acute redness, not to maintain a long‑term solution. If you need something stronger, a dermatologist might switch you to a medium‑strength Topical steroid such as triamcinolone or betamethasone, but those come with stricter monitoring.
In New Zealand, many pharmacies stock low‑dose hydrocortisone without a script, but the packaging will warn: “For short‑term use only. Do not exceed 14 days without medical advice.” That label is there for a reason, and we’ll see why in the next sections.
Potential Benefits for Redness and Inflammation
When you apply a thin layer of hydrocortisone to a rosacea flare, the most noticeable change is a reduction in Erythema the medical term for facial redness. Studies from 2023‑2024 show that low‑strength hydrocortisone can cut erythema scores by 30‑40 % after five days of consistent use.
Beyond the visible calm, patients often report less itching and burning. That relief is important because scratching can damage the skin barrier, leading to a vicious cycle of more inflammation. By soothing the itch, hydrocortisone indirectly helps the barrier heal.
One real‑world example: Sarah, a 42‑year‑old from Auckland, described a “worst‑case” flare that made her cheeks look sun‑burned for weeks. Her dermatologist prescribed a 1 % hydrocortisone cream for seven days, and she saw a noticeable fade in color and texture after the third day. She combined the steroid with a gentle moisturizer to keep her skin from drying out.
Side Effects and Risks You Should Know
Even though hydrocortisone is “low‑potency,” it isn’t risk‑free. The most common complaint is Skin thinning also called atrophy, where the skin becomes fragile and translucent. If you keep the cream on for longer than recommended, the epidermis can lose collagen, making tiny blood vessels more visible.
Another pitfall is “Steroid rebound a flare that returns stronger after stopping the steroid.” When the skin gets used to the drug, it may over‑react once the medication is withdrawn, leading to a cycle of repeated short courses.
Less common but still worth noting are perioral dermatitis (red bumps around the mouth) and telangiectasia (visible tiny veins). People with sensitive skin or a history of steroid misuse should be especially cautious.
Finally, because steroids suppress the local immune response, there’s a slight chance of secondary infection if the skin barrier is already broken. That’s why many dermatologists pair hydrocortisone with an antimicrobial or suggest a non‑steroidal alternative after the initial redness subsides.
How It Stacks Up Against Other Rosacea Treatments
Because every rosacea case is unique, doctors often choose a treatment based on the dominant symptoms-redness, bumps, or pustules. Below is a quick snapshot comparing the most common options.
| Feature | Hydrocortisone | Metronidazole | Azelaic Acid |
|---|---|---|---|
| Typical strength | 0.5‑2.5 % cream/gel | 0.75‑1 % cream | 15‑20 % gel |
| Primary target | Inflammation & erythema | Inflammation, papules | Redness, bumps, rosacea‑related acne |
| Onset of improvement | 2‑5 days | 1‑2 weeks | 2‑4 weeks |
| Common side effects | Skin thinning, rebound flare | Dryness, irritation | Burning, mild bleaching |
| Prescription needed? | Usually OTC for low strength | Prescription in NZ | Prescription in NZ |
If your main issue is a sudden flare of redness, hydrocortisone rosacea treatment can give you the fastest visible relief. For persistent papules or pustules, metronidazole or azelaic acid tend to work better over the long term. Some patients even rotate-starting with a short steroid burst, then maintaining with azelaic acid to keep the skin calm without the steroid’s downsides.
Practical Tips for Safe Use
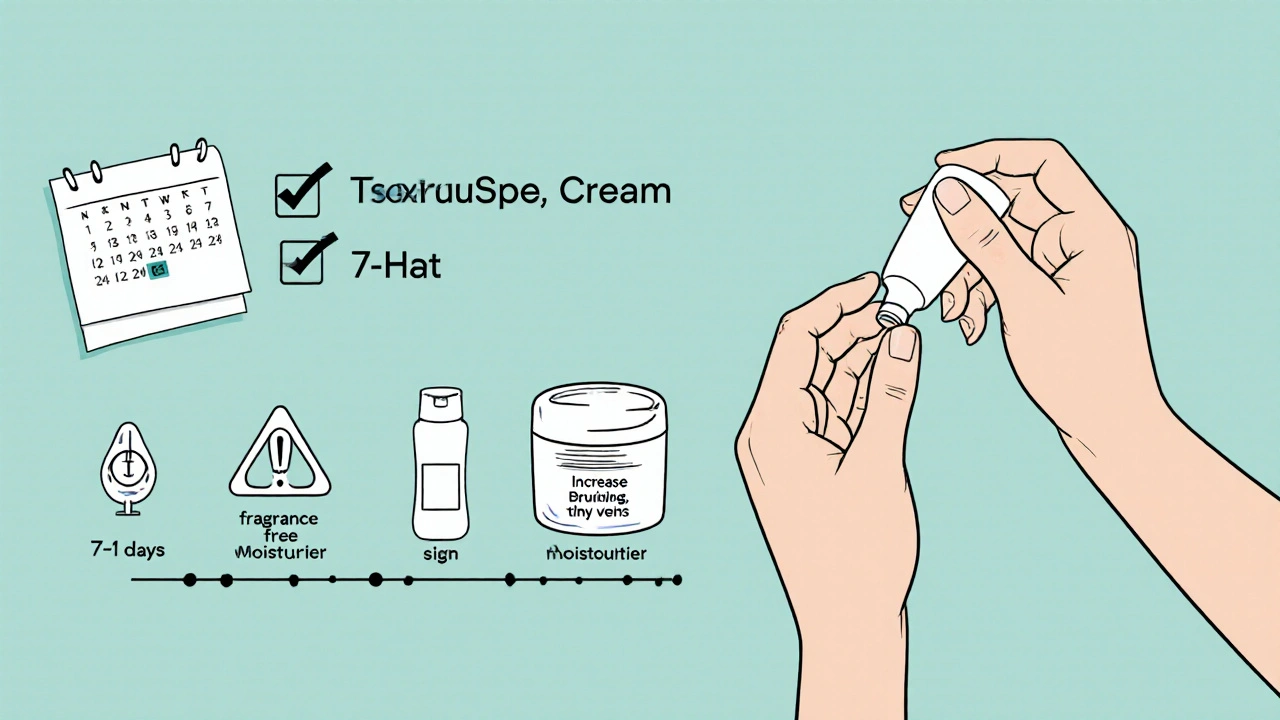
- Patch test: apply a pea‑sized amount to the inner forearm for 24 hours. If you see no irritation, it’s likely safe for facial use.
- Use a thin layer: Rub a small amount onto clean, dry skin. More isn’t faster.
- Limit duration: Stick to the 7‑14 day window unless your doctor advises otherwise.
- Moisturize afterward: A fragrance‑free moisturizer helps restore the skin barrier and reduces the risk of thinning.
- Avoid combining with other strong actives (e.g., retinoids or high‑strength acids) while the steroid is on your skin.
- Watch for warning signs: If you notice increased bruising, persistent burning, or new tiny veins, stop and call your dermatologist.
Remember, hydrocortisone is a tool-not a cure. Long‑term rosacea management usually involves gentle skin care, sun protection, and sometimes oral medications like Doxycycline an oral antibiotic with anti‑inflammatory properties for moderate to severe cases.
Frequently Asked Questions
Can I use hydrocortisone every day for rosacea?
Short‑term use (up to two weeks) is safe for most people. Daily use beyond that can thin the skin and trigger rebound flare. Talk to a dermatologist for a maintenance plan that doesn’t rely on steroids.
Is over‑the‑counter hydrocortisone strong enough?
For mild to moderate redness, a 1 % OTC cream often does the job. If you need faster or stronger results, a prescription‑strength formula may be recommended.
What should I do if my skin thins after using hydrocortisone?
Stop the steroid immediately and switch to a barrier‑repair moisturizer. A dermatologist can suggest alternatives like azelaic acid or low‑dose oral doxycycline to keep inflammation under control.
Can hydrocortisone worsen rosacea in the long run?
If used repeatedly or beyond the advised period, it can lead to steroid rebound, making flares more intense. That’s why it’s best saved for short bursts while you transition to other maintenance therapies.
Are there natural alternatives to hydrocortisone?
Yes. Ingredients like niacinamide, licorice extract, and green‑tea polyphenols have mild anti‑inflammatory effects. They work slower than steroids but are safe for daily use.
Bottom line: hydrocortisone can be a handy rescue for sudden rosacea redness, but it’s not a stand‑alone solution. Pair it with a solid skincare routine, sun protection, and-if needed-other prescribed treatments to keep your skin calm in the long run.




13 Comments
Look, we can't just slap a cheap steroid on our faces and expect miracles; it's a moral obligation to treat our skin responsibly, not to abuse pharmaceuticals like a teenager with a rebellious streak. If you keep reaching for the tube without consulting a dermatologist, you're basically endorsing a shortcut that will backfire with thinning skin and that dreaded rebound flare. It's not just about looking good for Instagram; it's about respecting the delicate barrier you were given.
Philosophically speaking, the transient relief offered by hydrocortisone invites us to contemplate the nature of impermanence – a brief calm before the inevitable return of the underlying inflammation. Yet, in practice, a short‑term course can be a pragmatic bridge to more sustainable therapies. :)
From a chill observer standpoint the low‑potency steroid serves as a quick‑acting anti‑inflammatory module its mechanism is basically glucocorticoid receptor binding reducing cytokine cascade minimal side‑effects when used within therapeutic window jargon‑heavy but effective
Hey, I totally get the appeal of a fast fix, but it's worth noting that pairing hydrocortisone with a gentle, fragrance‑free moisturizer can mitigate the risk of barrier disruption. Also, keep an eye on the duration – two weeks tops – and consider rotating to azelaic acid or a low‑dose oral doxycycline for maintenance. This balanced approach helps you reap the anti‑inflammatory benefits while preserving skin health.
Okay, guys, let’s keep it friendly – if you’re trying hydrocortisone, do a patch test first, and remember to moisturize afterward!!! That simple step can really cut down on that scary‑looking skin thinning later on. 🌿
Y’all, think of this like a sprint, not a marathon – the steroid is your burst of speed, but you gotta have a solid endurance plan (like a good barrier cream) to finish strong. Keep it colorful and stay consistent with sunscreen, and you’ll see those flames die down without the drama of rebound.
Honestly this whole "just use over‑the‑counter" thing is overrated. If you dont follow the 2 week limit youre gonna end up with skin thats as thin as paper and more visible veins. Stop messing around and get a proper consult.
sure hydrocortisone works but it also makes you dependent on steroids
Yo, from a cultural angle, many folks down under swear by that 1% cream as a quick rescue, but remember it’s a double‑edged sword – the aggressive approach can shut down inflammation while also ramming the skin’s natural defenses. Use it wisely, or you’ll pay the price in the form of rebound flare‑ups that feel like a busted pipe.
Drama alert! I once tried the cream for a whole week and woke up looking like a haunted Halloween prop – the redness vanished only to be replaced by ghostly translucent skin. It was a terrifying reminder that shortcuts in skincare can turn you into a walking cautionary tale.
Let's keep it respectful; use the steroid sparingly, watch for signs of thinning, and seek professional guidance if anything feels off – it's better to be safe than sorry.
When we talk about hydrocortisone in the context of rosacea management, we must first acknowledge the epistemological underpinnings that drive both clinical practice and consumer perception. The prevailing narrative-that a low‑potency corticosteroid can act as a panacea for acute erythema-offers a seductive simplicity that belies the complex pathophysiology of cutaneous vascular dysregulation and immune dysbiosis. In reality, hydrocortisone functions as a glucocorticoid receptor agonist, attenuating NF‑κB mediated transcription of pro‑inflammatory cytokines, thereby delivering a relatively rapid diminishment of edema and erythema. However, this mechanistic advantage is a double‑edged sword; chronic exposure precipitates dermal atrophy, loss of collagen fibrils, and a paradoxical upregulation of inflammatory mediators upon withdrawal-a phenomenon known as rebound flare. Consequently, the therapeutic window is critically narrow, often limited to a 7‑14 day regimen, after which a tapering protocol or adjunctive barrier repair strategy becomes imperative. Moreover, the integration of hydrocortisone into a multimodal treatment schema must consider patient‑specific variables such as skin type, rosacea phenotype, and comorbid sensitivities. For instance, individuals with predominant papulopustular lesions may derive less benefit than those with vascular predominance. In such cases, agents like metronidazole or azelaic acid, which target microbial colonization and keratinocyte turnover, respectively, become more appropriate first‑line therapies. Additionally, the psychosocial dimension of rosacea-often manifested as heightened self‑consciousness and social withdrawal-necessitates a compassionate approach that balances rapid symptomatic relief with long‑term skin health. Patient education about the potential for steroid‑induced skin thinning, telangiectasia, and perioral dermatitis is essential to foster informed consent and adherence to the prescribed regimen. Finally, the advent of novel non‑steroidal anti‑inflammatory topical agents, including brimonidine and oxymetazoline, offers promising alternatives that circumvent the adverse effect profile inherent to corticosteroids. Thus, while hydrocortisone remains a valuable tool in the dermatologic armamentarium for emergent rosacea flares, its deployment should be judicious, temporally constrained, and integrated within a broader, evidence‑based treatment algorithm.
Oh sure, because slapping a steroid on your face is the ultimate skincare hack-just ignore all the evidence and keep going, what could possibly go wrong?