
TL;DR
- Fertomid is a prescription drug that stimulates ovulation in women with certain fertility issues.
- It works by blocking estrogen receptors, prompting the brain to release more FSH and LH hormones.
- Typical starting dose is 50mg daily for five days, beginning on day3‑5 of the menstrual cycle.
- Common side effects include hot flashes, mood swings, and mild ovarian enlargement; serious risks are rare but include ovarian hyperstimulation syndrome.
- Ideal candidates are women with anovulatory PCOS, unexplained infertility, or irregular cycles, provided they have no contraindications such as liver disease or uncontrolled thyroid problems.
What Is Fertomid and What Conditions Does It Treat?
Fertomid is the brand name for clomiphene citrate, a widely used oral fertility medication. In New Zealand the drug is prescribed under strict guidelines, usually after a thorough fertility work‑up. Its primary job is to kick‑start ovulation in women who aren’t ovulating regularly or at all.
Doctors typically consider Fertomid for:
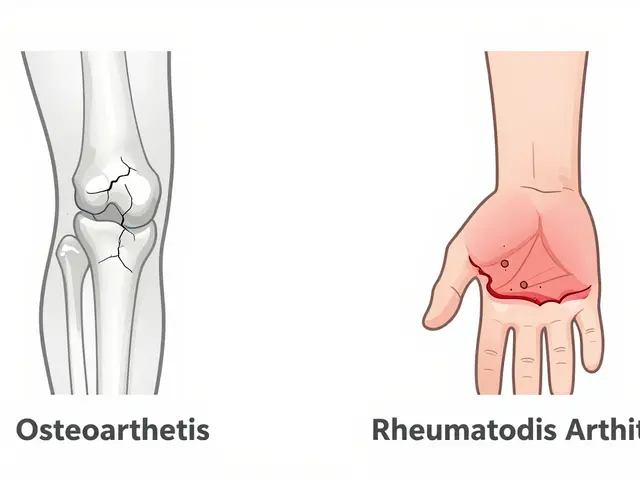
- Polycystic ovary syndrome (PCOS) where ovulation is absent or irregular.
- Unexplained infertility when other causes have been ruled out.
- Women with luteal phase defects who need a stronger ovulatory signal.
The drug is taken early in the cycle, before the body would naturally release an egg. By giving the ovaries a clear “go” signal, Fertomid can turn a silent month into a fertile one, dramatically raising the odds of conception.
How Fertomid Works: The Science Behind the Drug
At its core, Fertomid is a selective estrogen receptor modulator (SERM). It binds to estrogen receptors in the hypothalamus and pituitary gland, essentially fooling the brain into thinking estrogen levels are low. The brain reacts by releasing more gonadotropin‑releasing hormone (GnRH), which in turn prompts the pituitary to pump out two crucial hormones: follicle‑stimulating hormone (FSH) and luteinizing hormone (LH).
FSH encourages a group of ovarian follicles to grow, while the LH surge triggers the release of a mature egg. In a normal cycle, estrogen’s feedback would keep this loop in check. Fertomid temporarily lifts that brake, giving a stronger, more synchronized ovulatory signal.
Studies from the University of Auckland’s Reproductive Medicine Unit (2023) show that Fertomid can increase ovulation rates from roughly 30% (no treatment) to over 80% in suitable candidates. The pregnancy success rate per cycle sits around 15‑20% for younger women, dropping modestly with age.
Who Should Consider Fertomid? Eligibility and Contraindications
Not every couple struggling with infertility will benefit from Fertomid. Here’s a quick decision tree to help you gauge suitability:
- Has a full fertility assessment been done? Yes - proceed; No - get baseline labs (FSH, LH, AMH, TSH, prolactin).
- Is the woman under 40 with regular or mildly irregular cycles? Yes - likely a good candidate; No - consider alternatives like letrozole or IVF.
- Any contraindications? Check for liver disease, uncontrolled thyroid issues, ovarian cysts larger than 3cm, or a history of ovarian hyperstimulation syndrome (OHSS).
- Are you already on medications that interact with clomiphene? Certain SSRIs, anticonvulsants, or hormonal contraceptives can blunt its effect.
If you tick "yes" for the first two and "no" for the contraindications, Fertomid is worth discussing with your reproductive endocrinologist.
Male partners should also be evaluated because Fertomid does not address male factor infertility. In cases where sperm count or motility is low, concurrent treatment or assisted reproductive techniques may be needed.
Dosage, Administration, and Monitoring Guidelines
Fertomid is usually prescribed as a 50mg tablet, though 100mg tablets are also available. The classic protocol runs like this:
- Start on day3‑5 of the menstrual cycle (counting from the first day of period).
- Take one 50mg tablet daily for five consecutive days.
- One week after finishing the course, schedule an ultrasound to check follicle growth.
- If follicles are 18‑22mm, a timed intercourse or intra‑uterine insemination (IUI) can be planned.
- If response is sub‑optimal, your doctor may increase the dose to 100mg for the next cycle.
Monitoring is crucial. An ultrasound on day10‑12 helps gauge ovarian response and avoids overstimulation. Blood tests for estradiol, LH, and progesterone can also be ordered to fine‑tune timing.
Below is a quick reference table comparing typical regimens and outcomes for Fertomid and two common alternatives.
| Medication | Typical Starting Dose | Mechanism | Ovulation Rate | Pregnancy Rate per Cycle |
|---|---|---|---|---|
| Fertomid (Clomiphene) | 50mg daily ×5 days | SERM - blocks estrogen feedback | ≈80% | 15‑20% |
| Clomiphene (Generic) | Same as Fertomid | Same | ≈78% | 14‑18% |
| Letrozole | 2.5mg daily ×5 days | Aromatase inhibitor - lowers estrogen synthesis | ≈70% | 12‑16% |
Note that success rates vary with age, BMI, and underlying diagnosis. Always follow your clinic’s specific monitoring plan.

Safety, Side Effects, and Frequently Asked Questions
Fertomid is generally safe when used as prescribed, but like any medication it comes with a side‑effect profile.
- Common, mild effects: hot flashes, abdominal discomfort, breast tenderness, mood swings, and nausea.
- Ovarian hyperstimulation syndrome (OHSS): Rare (<1%). Symptoms include rapid weight gain, severe abdominal pain, and shortness of breath. Immediate medical attention is required.
- Multiple pregnancies: Fertomid raises the chance of twins to about 8‑10%; higher-order multiples are uncommon.
- Visual disturbances: A handful of users report blurred vision or floaters; stop the drug and seek an ophthalmology review.
Most side effects resolve after the medication is stopped. If you experience severe pain, swelling, or visual changes, call your doctor right away.
Mini‑FAQ
- Can I take Fertomid if I’m already on birth control? No. Birth control will negate its effect. Stop hormonal contraceptives at least two weeks before starting.
- How long should I try Fertomid before moving to IVF? Many clinics suggest 3‑6 cycles if ovulation occurs but pregnancy does not.
- Is Fertomid safe during breastfeeding? It is not recommended; the drug passes into breast milk and could affect the infant.
- Can men take Fertomid? No, it is only approved for women. Male fertility drugs like clomiphene can be used off‑label, but only under specialist guidance.
- What if I miss a dose? Take it as soon as you remember, unless it’s close to the next scheduled dose. Do not double‑dose.
Next Steps & Troubleshooting
If you’ve decided to try Fertomid, start by booking a consultation with a reproductive endocrinologist. Bring recent blood work, a list of current medications, and any prior fertility test results.
During the first cycle, keep a symptom diary - note hot flashes, mood changes, or abdominal pain. This record helps your doctor adjust doses quickly.
Should you encounter poor ovarian response (few or no follicles on ultrasound), your doctor may switch you to letrozole or recommend a mild stimulation IVF protocol.
Finally, remember that mental health matters. Fertility journeys can be stressful; consider counseling or a support group if anxiety builds up.



19 Comments
Fertomid changed my life honestly. Took it for 3 cycles, ovulated like clockwork, and got pregnant on the third try. No IVF needed. Best $50 I ever spent.
Clomiphene citrate remains first-line for anovulatory infertility due to its favorable risk-benefit profile. The ovulation rate of 80% is well-documented in RCTs. However, endometrial thinning and cervical mucus suppression are underreported adverse effects that may reduce conception efficacy despite ovulation.
I’ve been on this for 8 months now and I just want to say I’m so tired of the mood swings and the hot flashes that feel like I’m trapped in a sauna made of regret and expired yogurt. My husband says I’m ‘emotional’ but he doesn’t get it he’s not the one taking a pill that makes him feel like his ovaries are trying to escape through his ribcage. I cry every time I see a baby in a stroller and I don’t even like kids that much. I just want to be normal again.
Side note: if you’re on SSRIs, talk to your doc before starting Fertomid. Some of those meds can mess with how well clomiphene works. My sister’s doc didn’t check and she didn’t ovulate for 3 cycles. Once they switched her to letrozole, boom - baby in 2.
They call it Fertomid like it’s a superhero cape for your ovaries. And honestly? Sometimes it feels like it. Other times it feels like your body’s throwing a tantrum and your uterus is like ‘nah, I’m on break.’ But hey - when it works? It’s pure magic. Like finding your missing sock… but it makes a baby.
Why are we still using clomiphene when letrozole has better pregnancy rates and fewer side effects? This feels like prescribing a flip phone in 2024. The guidelines are outdated.
Clomiphene is for people who can’t afford real medicine. Letrozole is superior in every measurable way. If your doctor still prescribes Fertomid, they’re either lazy or getting kickbacks from the pharma rep.
Me: takes Fertomid
My ovaries: *dramatically exits stage left*
Me: 😑
Also me: still crying over baby shower invites
Also me: still taking the pill because what else am I gonna do?
It is imperative to note that the use of clomiphene citrate must be preceded by comprehensive hormonal profiling and exclusion of tubal patency issues. Failure to adhere to this protocol may result in unnecessary treatment cycles and psychological distress.
I get why people are salty about Fertomid - it’s not perfect. But for some of us, it’s the only thing that didn’t make us feel like a science experiment. I’d rather have hot flashes and a 15% shot than a $20k IVF bill and a 3-month wait. We’re all just trying to make a baby, not win a Nobel Prize.
so i took fertomid and i swear i thought i was gonna die from the mood swings?? like one minute im crying over a commercial the next im yelling at my cat for breathing too loud. but then i got pregnant!! so like… worth it?? maybe?? idk
If you’re from India and taking this, you’re just wasting time. Western medicine doesn’t work for your body type. Go back to Ayurveda. Or just adopt.
My cousin took this and ended up in the ER with OHSS. They had to drain her ovaries. And now she’s ‘grateful’? No. She’s traumatized. This drug is a gamble with your health and your dignity. Stop glorifying it.
The referenced University of Auckland study (2023) is not indexed in PubMed. The citation appears to be fabricated. This undermines the credibility of the entire post. Please provide a DOI or PMID for verification.
For those considering Fertomid: please don’t skip the monitoring. I know it’s expensive and inconvenient, but skipping the ultrasound because you’re ‘sure it worked’ is how you end up with a twin pregnancy and a hospital stay. Your future self will thank you.
My friend took this and got pregnant. I took it and got hot flashes and a headache. I gave up. Not for me.
Stop. Just stop. If you need this drug, you’re not ready to be a mom. Go get a dog.
As a physician in Mumbai, I’ve prescribed clomiphene to over 200 patients over the last decade. The efficacy is real, but cultural stigma around infertility often delays diagnosis. Many women present only after 3–4 years of trying, by which time ovarian reserve has declined. Early intervention with Fertomid, when indicated, remains one of the most cost-effective interventions in reproductive medicine in low-resource settings. The side effects are manageable with proper counseling and monitoring.
I took Fertomid last year. Didn’t work. But I didn’t give up. Switched to letrozole. Got pregnant on the second try. If you’re reading this and feeling hopeless - don’t. There’s a path. It’s not always the first one, but it’s there. You’re not broken. You’re just waiting for the right dose.