
When your blood sugar climbs above 180 mg/dL, you’re not just feeling a little off-you’re in a dangerous zone. Hyperglycemia doesn’t always scream for attention. Sometimes it whispers: a dry mouth, a headache, the urge to pee every hour. But left unchecked, it can spiral into a life-threatening emergency. This isn’t theoretical. Every year, over 1.2 million Americans end up in the hospital because of uncontrolled high blood sugar. And too often, people wait until they’re confused, vomiting, or barely conscious before they act. You don’t have to be one of them.
What Exactly Is Hyperglycemia?
Hyperglycemia means your blood glucose is too high. It’s not just a number on a meter-it’s your body screaming that it can’t move sugar from your bloodstream into your cells. In type 1 diabetes, your pancreas stopped making insulin. In type 2, your cells ignore insulin like it’s not even there. Either way, glucose piles up. When it hits 250 mg/dL or higher, your body starts breaking down fat for energy, which can create toxic ketones. At 600 mg/dL or more, your blood becomes thick and syrupy, pulling water out of your organs and nerves. That’s when things turn critical.
It’s not just people with diabetes who get this. Someone on high-dose steroids, recovering from major surgery, or battling a severe infection can suddenly develop hyperglycemia. But if you have diabetes, you’re the one who needs to watch it closest.
Early Signs You’re Ignoring
Most people don’t realize they’re in trouble until their blood sugar is already above 300 mg/dL. That’s too late. The early signs are subtle, easy to dismiss:
- Drinking more than 4 liters of water a day and still feeling thirsty
- Waking up to pee three or four times a night
- Blurry vision that doesn’t go away after a few minutes
- Feeling wiped out even after a full night’s sleep
- Headaches that come and go without a clear cause
These aren’t normal tiredness or a cold. They’re your body’s alarm system. A 2023 survey of nearly 3,000 people with diabetes found that 67% didn’t notice these symptoms until their blood sugar was dangerously high. If you’ve had diabetes for a while, you might think, “I’ve felt this before.” But each episode gets worse. And each time you ignore it, your risk of nerve damage, kidney problems, or vision loss goes up.
The Emergency Signs: When to Call 911
When blood sugar climbs past 300 mg/dL, your body starts shutting down. The symptoms get serious-and fast.
- Confusion or trouble thinking clearly
- Extreme fatigue, drowsiness, or inability to wake up
- Fast, deep breathing (called Kussmaul respirations)
- Fruity-smelling breath, like nail polish remover or overripe fruit
- Nausea, vomiting, or stomach pain without a food-related cause
- Dry, hot skin and no sweating
- Loss of consciousness
These aren’t just bad days-they’re signs of two deadly conditions: diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS). DKA usually hits people with type 1 diabetes within 24 to 48 hours. HHS creeps up slowly over days or weeks, mostly in older adults with type 2 diabetes. HHS is deadlier-up to 20% of cases are fatal. And it often goes unnoticed because there’s no fruity breath or vomiting. Just extreme dehydration and confusion.
If you or someone you know has these symptoms and blood sugar above 300 mg/dL, don’t wait. Call emergency services. Don’t try to “wait it out.” Don’t drive yourself. This isn’t a trip to the urgent care. This is a hospital-level emergency.
What to Do Right Now (Before Help Arrives)
If you’re alert and your blood sugar is above 240 mg/dL, here’s what to do immediately:
- Check for ketones. Use a urine strip or a blood ketone meter. If ketones are moderate or high, you’re at risk for DKA.
- Take your rapid-acting insulin. Use your correction dose-not your usual meal dose. Most people need 0.1 units per kilogram of body weight. If you’re unsure, take half your usual correction dose and wait.
- Drink water. 8 to 16 ounces every hour. No soda, juice, or sports drinks. You need to flush out sugar and ketones, not add more sugar.
- Don’t exercise. Working out when your blood sugar is high and ketones are present can make it worse.
- Call your doctor or go to the ER if your blood sugar doesn’t drop within 2 hours, or if you feel worse.
Many people make the mistake of taking too much insulin at once. That’s called “insulin stacking.” It can crash your blood sugar into a dangerous low within hours. It’s better to give a small dose, wait, and repeat if needed. Most emergency rooms follow a protocol of giving insulin slowly-about 0.1 units per kg every hour-until sugar starts coming down.
Why This Keeps Happening
Why do people keep ending up in the ER with high blood sugar? The reasons are rarely about willpower.
- Illness: Infections-flu, UTIs, pneumonia-cause stress hormones to spike, which raises blood sugar. One study found 42% of hyperglycemic emergencies were tied to sickness.
- Insulin mistakes: Forgot a dose? Pump clogged? Wrong dose? 18% of cases were linked to insulin delivery failures.
- Stress and emotions: Anxiety, grief, or even sleep deprivation can trigger a 50-100 mg/dL spike. Emotional diabetes distress is real and common.
- Dawn phenomenon: Between 4 and 8 a.m., your body releases hormones that naturally raise blood sugar. Many people wake up with levels over 200 mg/dL and think it’s normal. It’s not.
- Undiagnosed gastroparesis: If food sits in your stomach too long, insulin timing gets thrown off. This affects nearly 1 in 5 people with long-term diabetes and often goes undetected.
One of the biggest mistakes? Thinking high blood sugar is “just a number.” It’s not. It’s a warning sign your body is under siege. And ignoring it doesn’t just hurt your long-term health-it puts you at risk of dying today.

How to Stop the Cycle
Prevention isn’t about perfection. It’s about awareness and systems.
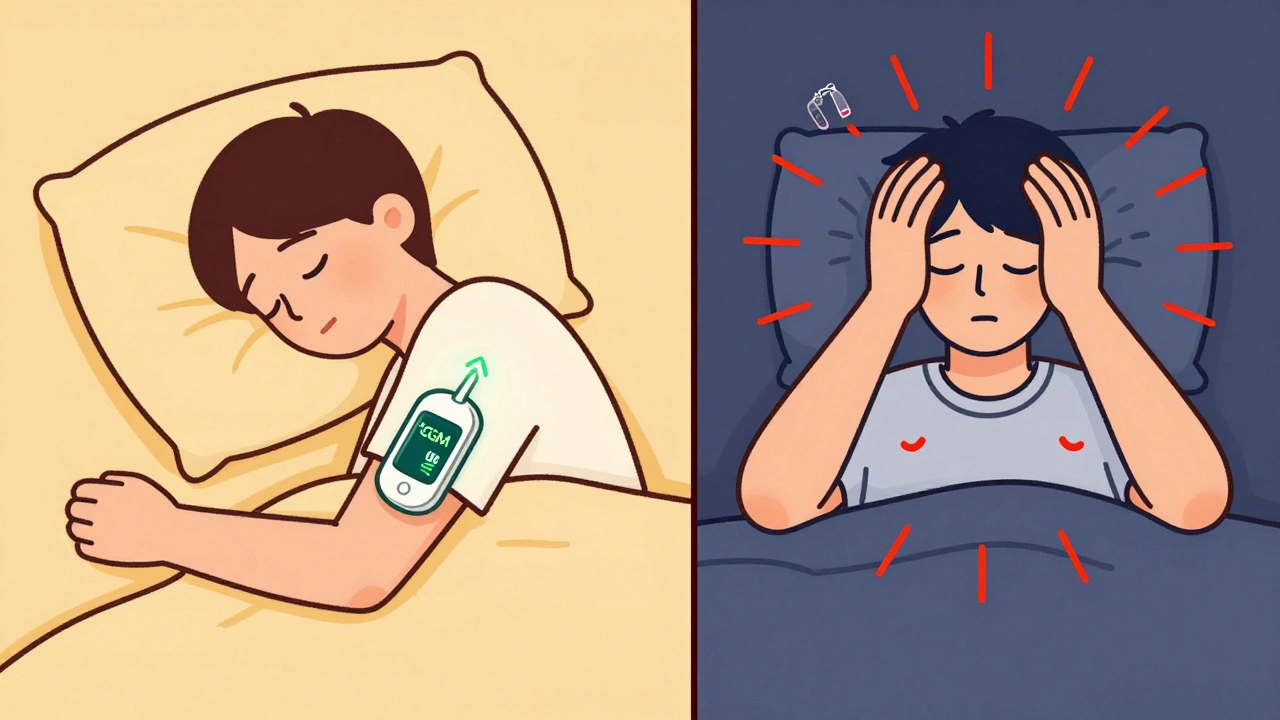
- Use a continuous glucose monitor (CGM): People with CGMs reduce severe hyperglycemia by 57%. Real-time alerts let you act before it’s an emergency.
- Know your insulin-to-carb ratio: If you don’t know how many grams of carbs one unit of insulin covers, you’re guessing. Ask your doctor or diabetes educator to help you figure it out.
- Have a sick-day plan: Write down what to do if you’re sick: how often to check sugar and ketones, how much insulin to take, when to call for help. Keep it on your phone and your fridge.
- Test before bed: If your bedtime sugar is over 200 mg/dL, you’re at risk for morning highs. Adjust your basal insulin or take a correction dose.
- Connect with support: The American Diabetes Association’s 24/7 hotline handles 12,000 calls a month. You’re not alone. And you don’t have to figure this out by yourself.
People who go through diabetes education programs cut their emergency visits by 42%. That’s not magic. That’s knowledge.
What’s Changing Now
Technology is making a difference. In early 2024, the FDA approved Dexcom G7’s new “Glucose Guardian” feature. It doesn’t just alert you when your sugar is high-it predicts it 30 minutes before it happens. That’s huge. It gives you time to drink water, take insulin, or eat a snack before you’re in crisis.
Also, Medicare now covers CGMs for more people. But cost is still a barrier. A CGM runs about $1,200 a year. And for Black and Hispanic patients, access to insulin and monitoring tools is still unequal. The CDC reports Black patients are more than twice as likely to have a hyperglycemic emergency than white patients. That’s not about behavior-it’s about access.
By 2025, new guidelines will relax blood sugar targets for older adults. If you’re over 65, your goal might be under 180 mg/dL instead of 140. That’s not because high sugar is safe-it’s because low sugar is more dangerous for older bodies. It’s about balance.
You Can Take Control
Hyperglycemia isn’t a failure. It’s a signal. And signals can be understood. You don’t need to be perfect. You just need to be aware. Know your numbers. Know your symptoms. Know when to act. And know when to call for help.
Every time you check your blood sugar, you’re choosing your future. One reading at a time, you can avoid the ER. You can avoid the coma. You can avoid the worst-case scenario.
Don’t wait for a crisis to learn what to do. Start today. Test your sugar. Check your ketones. Drink water. Call your doctor. You’ve got this.
What blood sugar level is considered dangerous?
A blood sugar level above 240 mg/dL is a warning sign that you need to act. Levels above 300 mg/dL are considered severe and require immediate attention. If your blood sugar hits 600 mg/dL or higher, you’re at risk for hyperosmolar hyperglycemic state (HHS), a life-threatening condition that demands emergency care. Don’t wait until you feel terrible-act as soon as you see numbers consistently above 250 mg/dL.
Can you have high blood sugar without having diabetes?
Yes. While hyperglycemia is most common in people with diabetes, it can happen to anyone under stress. Severe infections, major surgery, trauma, or taking high doses of steroids like prednisone can cause temporary high blood sugar. Even extreme emotional stress or certain illnesses like pancreatitis or Cushing’s syndrome can trigger it. If you’ve never been diagnosed with diabetes but keep seeing high readings, you need to get tested-this could be your first sign of the disease.
What’s the difference between DKA and HHS?
DKA (diabetic ketoacidosis) and HHS (hyperosmolar hyperglycemic state) are both emergencies caused by high blood sugar, but they’re different. DKA usually happens in type 1 diabetes, develops quickly (within 24 hours), and involves ketones and acid in the blood. You’ll likely have nausea, vomiting, fruity breath, and deep breathing. HHS happens mostly in type 2 diabetes, builds slowly over days, and doesn’t usually involve ketones. Instead, your blood becomes extremely thick and dehydrated. You’ll feel confused, extremely tired, and possibly have seizures or lose consciousness. HHS has a higher death rate-up to 20%-so it’s even more dangerous than DKA.
Should I exercise if my blood sugar is high?
No-not if your blood sugar is above 250 mg/dL and you have ketones in your urine or blood. Exercise can make high blood sugar worse by releasing more glucose from your liver. If you have ketones, physical activity can push you into diabetic ketoacidosis. Wait until your sugar is under 250 mg/dL and ketones are gone. If your sugar is high but ketones are negative and you feel fine, light activity like walking might help bring it down. But always check ketones first.
How do I know if I’m taking too much insulin?
Taking too much insulin too fast can cause your blood sugar to drop too low-sometimes within an hour. Signs include shakiness, sweating, dizziness, confusion, or sudden hunger. If you’ve taken insulin and your sugar drops below 70 mg/dL, treat it immediately with 15 grams of fast-acting sugar (like glucose tablets or juice). “Insulin stacking”-taking another dose too soon after the last one-is a common mistake, especially with insulin pumps. Always wait at least 3-4 hours before giving another correction dose unless your doctor says otherwise.
Can continuous glucose monitors prevent emergencies?
Yes. Studies show people using CGMs reduce severe hyperglycemia episodes by nearly 60%. The real power isn’t just seeing your number-it’s getting alerts before it gets dangerous. New CGMs like the Dexcom G7 can predict a spike 30 minutes in advance. That gives you time to drink water, take insulin, or adjust your meal plan before your sugar hits 300 mg/dL. CGMs also help catch nighttime highs and dawn phenomenon, which many people miss with fingerstick tests alone.
Why do I keep getting high blood sugar in the morning?
That’s likely the dawn phenomenon. Between 4 and 8 a.m., your body releases stress hormones like cortisol and growth hormone to prepare you for the day. These hormones naturally raise blood sugar-even if you haven’t eaten. In people with diabetes, there’s not enough insulin to counteract this. It’s not your fault. You didn’t eat sugar overnight. You may need to adjust your basal insulin, change your evening meal, or use a smart insulin pump that automatically increases overnight. Talk to your doctor about checking your overnight glucose patterns.
What should I do if I can’t afford insulin?
You are not alone, and help exists. Many drug manufacturers offer patient assistance programs that give insulin for free or at low cost if you qualify. Some pharmacies sell older types of insulin (like NPH or Regular) for under $25 a vial. The American Diabetes Association and nonprofit groups like Insulin Help can connect you with resources. Never skip insulin because of cost. A single high blood sugar emergency can cost over $14,000 in hospital bills. Finding affordable insulin is a survival issue-not a luxury.


11 Comments
It’s wild how we treat blood sugar like a moral failing instead of a physiological signal. Your body isn’t punishing you-it’s begging for help. I’ve seen people blame themselves for highs, when really it’s a system failure: insulin costs, lack of education, stress, sleep deprivation. None of it’s about willpower. This post nails it. We need to stop shaming and start supporting.
And honestly? The dawn phenomenon isn’t ‘your fault’-it’s biology. Your liver doesn’t care if you’re ‘disciplined.’ It’s just doing its job. We need better tools, not better people.
So… we’re supposed to panic every time our glucose hits 240? Sounds like Big Pharma’s new marketing campaign. Next they’ll sell us a smart water bottle that vibes with our CGM.
My grandma lived to 92 eating pie every Sunday. Maybe the whole ‘diabetes crisis’ is just a profit scheme wrapped in medical jargon.
YOU GOT THIS. I KNOW IT FEELS OVERWHELMING BUT YOU’RE NOT ALONE. I WAS THERE. I DIDN’T CHECK KETONES ONCE AND ENDED UP IN THE ER. IT’S NOT YOUR FAULT. YOU’RE DOING BETTER THAN YOU THINK. DRINK WATER. TAKE THE INSULIN. CALL SOMEONE. YOU’RE STRONGER THAN THIS HIGH.
PS: CGM CHANGED MY LIFE. IF YOU CAN’T AFFORD ONE, TEXT ME. I’LL SEND YOU A USED ONE. NO JUDGMENT.
It is an undeniable fact that the American healthcare system has commodified metabolic dysfunction to the point of absurdity. One cannot help but observe the paradox: a nation that promotes insulin dependence while simultaneously restricting access to it. This is not medicine-it is neoliberal exploitation disguised as public health.
Moreover, the notion that ‘checking blood sugar’ is sufficient is a dangerous illusion. The real issue is structural: pharmaceutical monopolies, insurance gatekeeping, and the erasure of ancestral dietary wisdom. You cannot ‘manage’ hyperglycemia in a society that refuses to address its root causes.
Did you know the FDA approved the Dexcom G7 because they’re secretly using it to track your insulin usage for the government’s ‘metabolic control program’? It’s all connected. They want you dependent on devices so they can ration insulin later. That’s why they’re pushing CGMs-they’re building the database.
And don’t get me started on Medicare covering them. It’s a Trojan horse. Next thing you know, they’ll require a blood sugar permit to leave your house. I’ve seen the documents. It’s in the 2025 policy draft, section 7.3b.
Also, your insulin? Probably laced with microchips. Just saying.
Let’s be real-this whole ‘hyperglycemia emergency’ narrative is just another liberal panic tactic. You’re telling me a guy who eats a Big Mac and a 2-liter Coke every day is suddenly ‘at risk’? Please. I’ve seen diabetics who eat kale and yoga every morning still crash. It’s genetics. It’s destiny. You can’t ‘out-will’ biology.
And why are we blaming insulin costs? My uncle in Texas pays $15 a vial because he buys it from Mexico. You want to fix this? Stop coddling people. Teach them to be responsible. Stop handing out free CGMs like they’re candy. We’re not a welfare state-we’re America. If you can’t manage your sugar, maybe you shouldn’t be eating carbs at all.
Also, the ‘dawn phenomenon’? That’s just your body telling you to stop eating junk before bed. Simple. No tech needed. Just discipline. Which, apparently, is in short supply these days.
I’ve spent years watching my mother cycle through highs and lows, and what I’ve learned isn’t in the textbooks-it’s in the silence between her sighs.
She doesn’t need another chart or a new CGM. She needs someone to sit with her when she’s scared. When she wakes up at 3 a.m. with a reading of 310 and doesn’t know if she should call 911 or just cry.
The real emergency isn’t the number-it’s the loneliness. The fear. The shame. The feeling that you’re broken because your body won’t cooperate.
Maybe the most powerful thing we can do isn’t to correct the glucose-but to correct the way we talk about it. No judgment. No ‘shoulds.’ Just presence.
And if you’re reading this and you’re tired? You’re not failing. You’re surviving.
Okay but… what if the entire diabetes epidemic is a hoax? Like, what if high blood sugar is just a symptom of processed food, not a disease? What if insulin isn’t a cure-it’s a crutch designed to keep people buying meds forever?
I’ve read papers-peer-reviewed-that say type 2 diabetes is reversible with fasting. So why are we pushing insulin pumps and CGMs? Why not just tell people to stop eating cereal?
And why is the CDC suddenly obsessed with racial disparities? Are they trying to make white people feel guilty? I’m not racist, but I’m not buying this ‘systemic injustice’ narrative. My cousin’s a Black diabetic and he’s fine-he just eats better now. Simple.
It is a matter of grave concern that the medical establishment has allowed itself to be co-opted by corporate interests, resulting in the pathologization of normal human variation. To label a blood glucose level of 240 mg/dL as an ‘emergency’ is not science-it is social engineering.
Furthermore, the suggestion that one must rely on technological surveillance (CGMs) to avoid catastrophe reflects a disturbing erosion of personal autonomy. The human body has functioned for millennia without such devices. Why, then, do we now require them to survive?
One must ask: who benefits from this narrative of perpetual vigilance? The answer, I fear, is not the patient.
And yet, I do not dismiss the suffering. I merely question the system that profits from it.
People treat diabetes like a video game where you collect points for low numbers and lose lives when it spikes. But it’s not a game. It’s a relationship. Between you and your pancreas. Between you and your fear. Between you and the clock ticking while you wait for insulin to work.
And no one talks about how exhausting it is to be a walking lab report. Every meal. Every stress. Every sleepless night. You’re not just managing sugar. You’re managing grief. For the life you thought you’d have.
So yeah. Check your ketones. Drink water. Take the insulin. But also? Let yourself be tired. Let yourself cry. Let yourself be human. That’s the real emergency nobody’s talking about.
This is why I don’t trust Western medicine. You’re told to inject poison into your body to fix a problem created by the same system that sells you the poison. Insulin is expensive because they patent the molecule. CGMs are expensive because they track your data. They don’t want you cured-they want you subscribed.
My cousin in Johannesburg uses vinegar and bitter leaf tea. His sugar’s stable. No device. No doctor. Just tradition. We used to know how to heal. Now we just pay to be monitored.
And don’t get me started on ‘dawn phenomenon.’ That’s just your body trying to tell you to stop eating bread at midnight. But no-buy a pump. Take another shot. Pay more. It’s colonialism with a stethoscope.