
Antibiotic Sun Safety Calculator
Sun Sensitivity Risk Calculator
Your Sun Sensitivity Risk
Essential Protection: UPF 30+ clothing, wide-brimmed hat, SPF 30+ broad-spectrum sunscreen.
When you’re prescribed doxycycline or TMP-SMX (Bactrim, Septra), your doctor focuses on killing the infection. But there’s another, less talked about side effect that can turn a sunny day into a painful mistake: photosensitivity. It’s not just about getting a little tan. This reaction can burn your skin in under an hour-even through a window-and stick around long after you’ve finished your pills.
What Exactly Is Antibiotic Photosensitivity?
Photosensitivity means your skin reacts badly to sunlight because of a drug. It’s not an allergy in the usual sense. Instead, the antibiotic molecules in your skin absorb UV light and turn it into something harmful. This triggers a chemical reaction that damages your skin cells. About 95% of these reactions are phototoxic, meaning they look like a bad sunburn: red, hot, painful, sometimes blistering. The rest are photoallergic, which show up days later as an itchy, eczema-like rash. Both are preventable. Most people don’t know they’re at risk until it’s too late.Why Doxycycline and TMP-SMX Are High Risk
Not all antibiotics cause this. Penicillin? Almost never. But doxycycline and TMP-SMX are among the worst offenders. Studies show that about 20% of people taking doxycycline at standard doses (200 mg daily) will get a phototoxic reaction. In some cases, even one hour of sun exposure can trigger it. Demeclocycline, another tetracycline, is even worse-up to 9 out of 10 patients developed burns in clinical trials. TMP-SMX works differently. Its active ingredient, sulfamethoxazole, absorbs a broader range of UV light. That means you can get burned even on cloudy days or near a window. What’s worse? The reaction can last for weeks after you stop taking it. One patient I spoke with got a severe burn two weeks after finishing Bactrim for a UTI. She thought she was safe because she was off the pills. She wasn’t.How UV Light Triggers the Reaction
The sun’s rays aren’t all the same. UVB (290-310 nm) causes sunburns. UVA (320-400 nm) penetrates deeper and causes aging. But here’s the catch: doxycycline absorbs UVA. That’s why you can get burned inside your car, in your kitchen by the window, or walking to the mailbox. Standard window glass blocks UVB but lets UVA through. So if you’re on doxycycline, sitting by a sunny window isn’t safe. TMP-SMX reacts to both UVA and UVB. This makes it harder to avoid. Even brief exposure-like stepping outside to grab the mail-can be enough. Studies show the minimum dose of UV needed to burn skin drops by up to 50% in people taking these antibiotics. That means your skin burns at half the sun exposure you’d normally tolerate.How Long Do You Need to Stay Protected?
This is where most people get it wrong. For doxycycline, you need sun protection for the entire time you’re taking it-and for about 3-5 days after your last dose. The drug clears from your system fairly quickly. For TMP-SMX? It’s different. The sulfamethoxazole component lingers in your skin. Experts at the Skin Cancer Foundation and medical sources confirm: you can still burn weeks after stopping Bactrim. One study tracked patients for 14 days after discontinuation and still saw elevated sun sensitivity. That means if you’re planning a beach trip two weeks after finishing your pills, you’re not in the clear.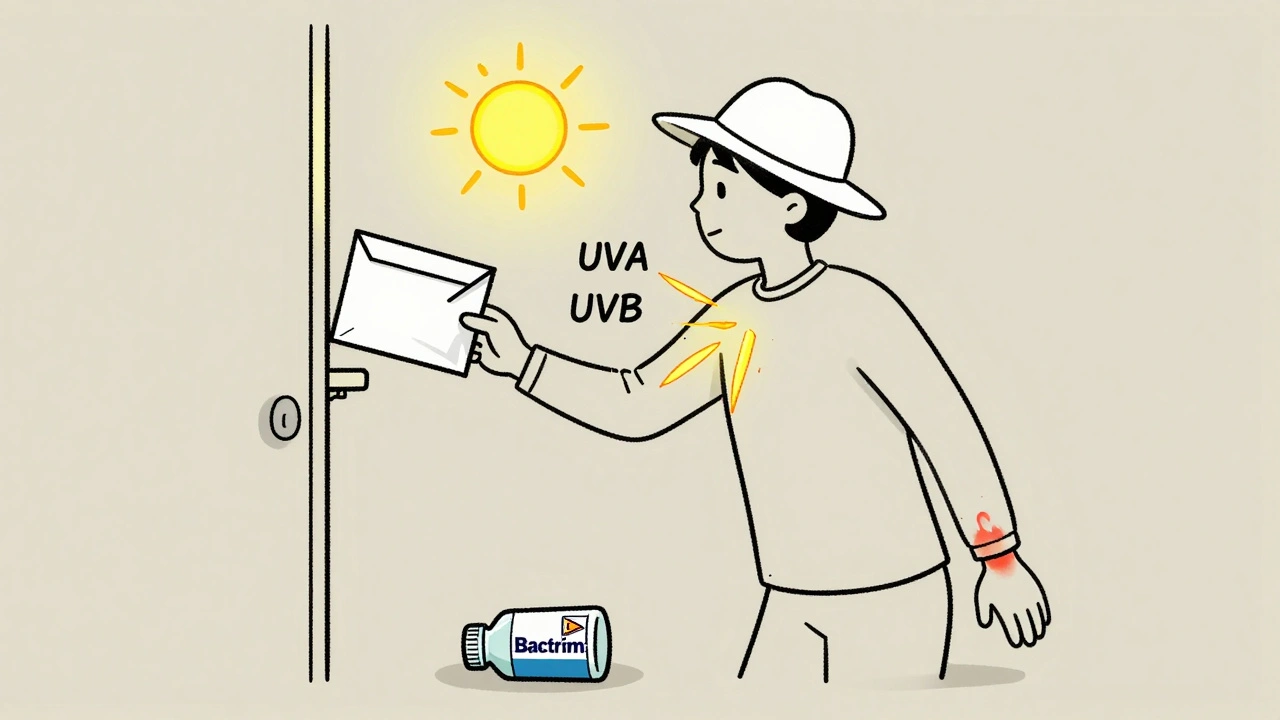
What Sun Protection Actually Works
Saying “wear sunscreen” isn’t enough. You need a full strategy.- Sunscreen: Use broad-spectrum SPF 30 or higher. Reapply every two hours, even if you’re not sweating. Look for zinc oxide or titanium dioxide-they physically block UVA better than chemical filters.
- Clothing: Regular cotton T-shirts only offer UPF 5-10. That’s not enough. Wear UPF 30+ sun-protective clothing. Long sleeves, wide-brimmed hats, and UV-blocking sunglasses make a real difference.
- Timing: Avoid direct sun between 10 a.m. and 4 p.m. That’s when UV intensity peaks. Even short walks during these hours can trigger a reaction.
- Indoors: If you sit near a window at home or in the office, you’re still exposed. UVA passes through glass. Consider UV-blocking window film or stay away from sunny spots.
What Doesn’t Work
Many people think they’re safe if they don’t get “burned.” But photosensitivity doesn’t always look like a classic sunburn. It can be a rash, peeling skin, or dark patches that last for months. Some patients report permanent hyperpigmentation after one bad reaction. Also, don’t rely on “water-resistant” sunscreen. Sweat, towels, and time break it down. Reapplication is non-negotiable. And no, tanning beds are not a workaround. They emit intense UVA-exactly the kind that triggers these reactions. Skip them entirely while on these antibiotics.Why Doctors Don’t Always Warn You
Here’s the uncomfortable truth: many healthcare providers don’t emphasize this risk. A 2023 review found that nearly 40% of patients on doxycycline or TMP-SMX received no sun safety advice at all. Some think it’s “just a minor side effect.” But it’s not. Severe phototoxic reactions can lead to blistering, infection, and scarring. And if you stop your antibiotics early because of the pain, you risk antibiotic resistance or a recurring infection. The FDA has required sun safety warnings on doxycycline and TMP-SMX packaging since the early 2000s. But that doesn’t mean patients see it. Medication guides get lost. Prescriptions get filled. Advice gets lost in translation.What to Do If You Get Burned
If you notice redness, pain, or blistering within hours of sun exposure:- Get out of the sun immediately.
- Cool the area with damp cloths-no ice.
- Use aloe vera or hydrocortisone cream (1%) to reduce inflammation.
- Take ibuprofen to ease pain and swelling.
- Don’t pop blisters. That increases infection risk.
- Contact your doctor if the burn covers a large area, blisters badly, or doesn’t improve in 48 hours.
Long-Term Risks You Can’t Ignore
This isn’t just about a bad day at the beach. Repeated phototoxic reactions damage your skin’s DNA. Over time, that increases your risk of skin cancer. The Skin Cancer Foundation links chronic sun exposure during antibiotic use to higher rates of squamous cell carcinoma. You’re already taking a powerful drug. Don’t stack another risk on top.Final Advice: Treat It Like a Prescription
Sun protection isn’t optional when you’re on doxycycline or TMP-SMX. It’s part of your treatment plan. Just like you wouldn’t skip a pill, you shouldn’t skip sunscreen, a hat, or shade. Plan your days. Check the UV index. Wear protective gear. Tell your family what to watch for. The good news? If you follow these steps, you can take your antibiotics safely. You can live normally. You just need to be smarter about the sun.Can I still go outside if I’m taking doxycycline or Bactrim?
Yes, but you need to be extremely careful. Avoid direct sun between 10 a.m. and 4 p.m. Wear UPF 30+ clothing, a wide-brimmed hat, and broad-spectrum SPF 30+ sunscreen. Reapply sunscreen every two hours. Even indoors near windows, UVA rays can trigger a reaction, so sit away from direct sunlight.
How long after stopping Bactrim am I still at risk?
You can still be sensitive for up to two weeks after your last dose of TMP-SMX (Bactrim). The sulfamethoxazole component stays in your skin longer than the drug stays in your bloodstream. Don’t assume you’re safe just because you finished your pills. Keep using sun protection for at least 14 days after stopping.
Is SPF 15 enough if I’m on antibiotics?
No. SPF 15 blocks about 93% of UVB rays. But antibiotics like doxycycline and TMP-SMX make your skin far more sensitive to UVA, which SPF 15 doesn’t block well. Use SPF 30 or higher with broad-spectrum coverage (UVA/UVB). Look for zinc oxide or titanium dioxide as active ingredients-they offer the most reliable protection.
Do all antibiotics cause sun sensitivity?
No. Penicillins, cephalosporins, and macrolides like azithromycin rarely cause photosensitivity. But doxycycline, other tetracyclines, TMP-SMX, ciprofloxacin, and levofloxacin are high-risk. Always ask your pharmacist or doctor if your specific antibiotic can make your skin sun-sensitive.
Can I use tanning beds while on these antibiotics?
Absolutely not. Tanning beds emit concentrated UVA radiation-the exact type that triggers phototoxic reactions with doxycycline and TMP-SMX. Using one while on these drugs can cause severe burns, blistering, and long-term skin damage. There is no safe level of tanning bed use while taking these antibiotics.
Will sunscreen completely prevent a reaction?
Sunscreen reduces risk but doesn’t eliminate it. No sunscreen blocks 100% of UV rays. Combine it with protective clothing, shade, and avoiding peak sun hours. Think of sunscreen as one layer of defense-not your only one. Even with perfect sunscreen use, prolonged exposure can still cause a reaction if you’re highly sensitive.
What should I do if I develop a rash after sun exposure?
Stop sun exposure immediately. Apply cool compresses and a 1% hydrocortisone cream to reduce itching and inflammation. Take ibuprofen for pain. Avoid breaking any blisters. If the rash spreads, becomes painful, or doesn’t improve in 48 hours, contact your doctor. You may need a prescription steroid cream or to stop the antibiotic if the reaction is severe.



11 Comments
Man, I got burned bad on doxycycline last summer. Thought I was being careful-wore a shirt, sat under an umbrella. Nope. Window in my apartment turned my shoulders into a lobster. Took weeks to fade. Never thought about UVA through glass until now. Lesson learned.
Now I treat sunscreen like brushing my teeth. Every morning. No excuses.
This is the most comprehensive, clinically accurate breakdown of antibiotic photosensitivity I’ve ever read. The distinction between phototoxic and photoallergic reactions? Perfect. The 14-day window for TMP-SMX? Critical. Why isn’t this on every pharmacy handout?
Every provider who prescribes doxycycline or Bactrim should be required to read this before writing the script. This isn’t ‘minor’-it’s a preventable injury epidemic.
It’s fascinating how the pharmacokinetics of sulfamethoxazole create a dermal reservoir effect-persistent tissue concentration despite plasma clearance. This explains the delayed phototoxicity beyond the half-life. The skin isn’t just passive tissue here; it’s a bioactive substrate for photochemical reactions.
And yet, the clinical guidance remains woefully simplistic: ‘wear sunscreen.’ We need biomarkers, risk stratification, maybe even photopatch testing for high-risk patients. This isn’t just education-it’s a systems failure in pharmacovigilance.
you people are so soft. i took doxy in the desert with no protection and lived. you just wanna sit inside like babies. sun is good for you. stop being scared of everything. your skin will get tough if you stop whining.
While I acknowledge the pedagogical value of this exposition, I must register my profound dissatisfaction with the absence of referenced clinical trial data in the form of PubMed IDs, NIH trial registries, or FDA Adverse Event Reporting System (FAERS) case numbers. The assertion that '20% of people' experience phototoxicity is statistically meaningless without a confidence interval or sample size. This reads like a blog post masquerading as medical literature.
i had bactrim for a uti and went to the beach 10 days later. got burned so bad i cried. doc never said nothin. now i got dark spots that wont go away. why dont they tell you this stuff? its not like its secret. why do they just hand you the pill and send you on your way like a zombie?
OMG. I JUST REALIZED. I WAS ON DOXYCYCLINE AND WENT TO A MUSIC FESTIVAL. I WAS WEARING A WHITE T-SHIRT. I THOUGHT I WAS JUST 'TANNING.' I WASN'T. I WAS GETTING BIOLOGICALLY SCORCHED. I HAVE SCARS. I'M STILL ANGRY. WHY DID NO ONE WARN ME? THIS IS MEDICAL NEGLIGENCE. I'M STARTING A PETITION.
AND YES-I’M STILL WEARING A HAT. AND A COAT. INSIDE. BECAUSE I’M SCARED OF WINDOWS NOW.
bro this post is a lifesaver 🙏 i got burned so bad on doxy i thought i was dying. now i wear a hat indoors, sunscreen every day, and i even got UV-blocking window film for my car. no more regrets. also-tanning beds? nope. i’m not that dumb. 🌞🚫
thank you for writing this. seriously. you saved me from future dumb mistakes.
of course Americans are freaking out about sun. we have the best healthcare system in the world. if you can't handle a little UV, maybe you shouldn't be outside. in my country we just take the pill and go live. no sunscreen, no drama. you people need to toughen up.
Interesting how the phototoxic potential correlates with molecular absorption spectra-doxycycline’s peak at 355 nm aligns precisely with UVA transmission through standard glass. The fact that sulfamethoxazole’s half-life in dermal tissue exceeds plasma half-life by 300% suggests a sequestration mechanism in keratinocytes.
Yet the clinical response remains reactive rather than prophylactic. We need standardized risk scoring: age, skin type, duration of therapy, ambient UV index. A mobile app that auto-schedules sunscreen reapplication based on real-time UV data might reduce incidence by 60%.
Let us not mistake this as a simple matter of patient education. The systemic failure lies in the commodification of pharmaceutical care. Antibiotics are prescribed with the efficiency of fast food-dispensed, not discussed. The FDA warning label exists in a legalistic vacuum, disconnected from the human experience of care. The physician’s role has been reduced to a transactional gatekeeper, not a steward of holistic safety.
Furthermore, the normalization of photosensitivity as a 'minor' side effect reflects a broader cultural disregard for the body’s bioelectrochemical fragility. We treat the molecule, not the organism. And when the organism fails-when skin blisters, when pigmentation persists-we blame the patient for not reading the fine print. But the fine print was never meant to be read. It was meant to absolve.