Probiotic Timing Calculator
How to Use This Tool
Enter your antibiotic schedule below. Probiotics should be taken 2-3 hours after each antibiotic dose to maximize effectiveness.
The tool will calculate your optimal probiotic timing schedule. Always take probiotics with the recommended gap to avoid killing beneficial bacteria.
Recommended Probiotic Timing
Probiotics should be taken 2-3 hours after each antibiotic dose to maximize effectiveness.
Important Safety Information
Not suitable for:
- Immunocompromised individuals
- Those with central IV lines or artificial heart valves
- Recently hospitalized patients
- Patients with critical illness or on ventilators
Stop immediately if you experience fever, severe cramping, or bloody stool.
Key Strains for Antibiotic Therapy
| Strain | Effective for | Recommended Dose |
|---|---|---|
| Saccharomyces boulardii | Preventing C. difficile diarrhea | 500-1000 mg daily |
| Lactobacillus rhamnosus GG | Reducing antibiotic-associated diarrhea | 10 billion CFUs daily |
When you’re on antibiotics, you know the deal: the infection starts to clear up, but then your stomach turns against you. Diarrhea, bloating, cramps - it’s like your gut is staging a rebellion. That’s not just bad luck. Antibiotics don’t just kill the bad bacteria; they wipe out the good ones too. And when your gut microbiome gets knocked off balance, side effects follow. Around 1 in 5 people on antibiotics end up with antibiotic-associated diarrhea. For some, it’s mild. For others, it’s Clostridioides difficile infection - a serious, sometimes life-threatening condition that can land you in the hospital.
How Probiotics Help When You’re on Antibiotics
Probiotics are live bacteria and yeasts that are meant to support your gut health. They’re not magic pills, but they do have a clear job during antibiotic therapy: replace what antibiotics destroy. Think of your gut like a neighborhood. Antibiotics are like a citywide power outage - everything shuts down, including the helpful workers who keep digestion running and pathogens in check. Probiotics are the repair crew showing up with tools and fresh supplies.
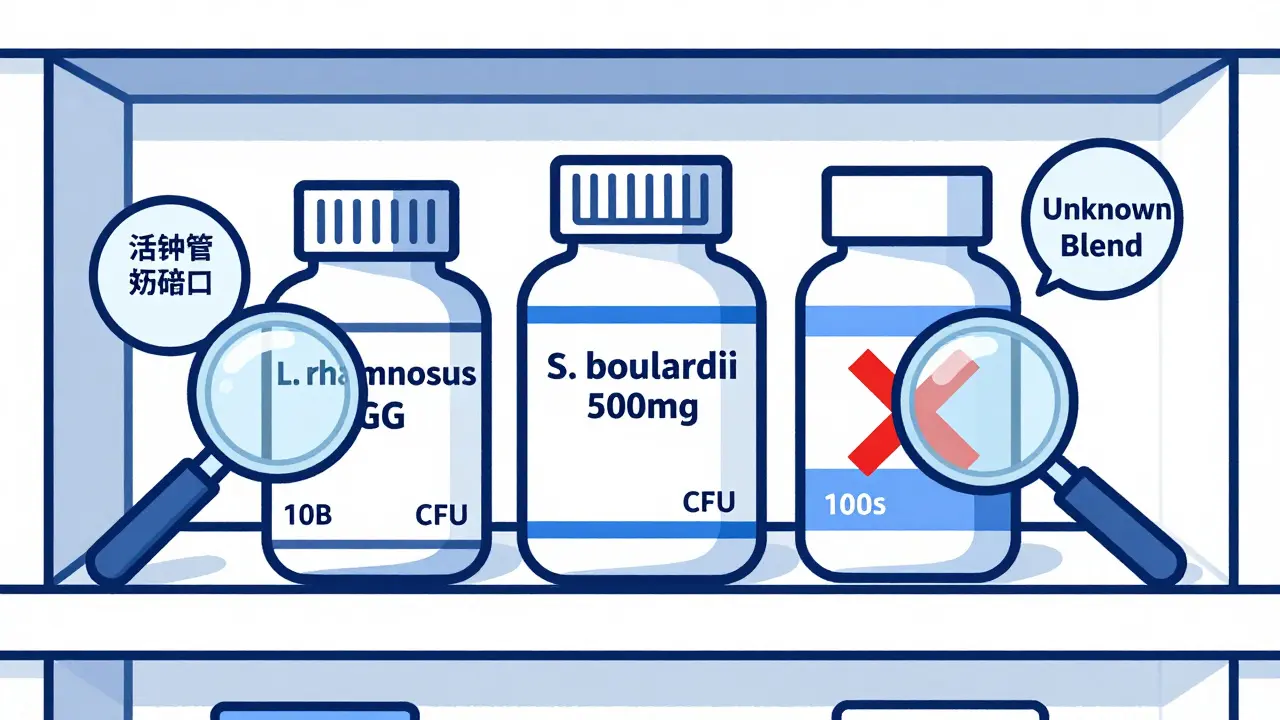
Not all probiotics are the same. The ones that actually work for antibiotic-related diarrhea have been studied hard. Two strains stand out: Lactobacillus rhamnosus GG and Saccharomyces boulardii. In clinical trials, S. boulardii cut the risk of antibiotic-associated diarrhea by about half. L. rhamnosus GG showed similar results, especially in kids and older adults. These aren’t just random bugs you find in yogurt - they’re specific, well-researched strains that survive stomach acid and stick around long enough to help.
How do they work? They crowd out harmful bacteria, produce substances that calm gut inflammation, and help restore the natural balance of your microbiome. They don’t stop antibiotics from doing their job. They just help your gut recover faster.
What the Science Actually Says
A 2020 Cochrane review - one of the most trusted sources in medical research - looked at 2454 people across 13 studies. The results were clear: if you’re at higher risk for severe diarrhea (like if you’re hospitalized or on strong antibiotics), taking probiotics cut your chance of getting C. difficile diarrhea from 11.6% down to 3.1%. That’s a 70% drop. That’s not a small benefit. That’s life-changing for some.
But here’s the catch: not all probiotics work the same. A mix of five different strains? Might do nothing. A single strain like L. rhamnosus GG? Might cut your risk by 60%. The evidence is strong for specific strains, weak for others. And while some studies say probiotics reduce overall side effects by 17%, others show no benefit at all. Why? Because many products on the shelf aren’t backed by science. You’re not just buying probiotics - you’re buying a specific strain, at a specific dose, from a brand that actually tested it.
And yes, there’s conflicting data. One 2021 study in Nature suggested that taking probiotics after antibiotics might actually slow down your natural microbiome recovery. That’s a red flag. It means probiotics aren’t a one-size-fits-all fix. For some people, they help. For others, they might just delay healing. That’s why timing and strain matter more than ever.
Which Probiotics Actually Work?
Forget the multi-strain blends with 20 different bacteria on the label. Most of those are marketing fluff. Stick to the ones with real data:
- Saccharomyces boulardii - a yeast, not a bacteria. Works well for preventing C. diff and traveler’s diarrhea. Dose: 500-1000 mg daily.
- Lactobacillus rhamnosus GG - the most studied strain. Found in Culturelle and other brands. Dose: 10 billion CFUs daily.
- Bifidobacterium lactis - helps with bloating and gas. Often paired with L. acidophilus.
- Streptococcus thermophilus - common in yogurt, but less effective alone for antibiotics.
Multi-strain products can work, but only if they include one of the proven strains above. Avoid anything that doesn’t list the exact strain names. If it just says “probiotic blend,” walk away. That’s not transparency - that’s guesswork.
How to Take Them - Timing Matters
Don’t take your probiotic at the same time as your antibiotic. Antibiotics kill bacteria - including the good ones you’re trying to replace. If you take them together, the antibiotic will kill the probiotic before it even gets to your gut.
The best practice? Take your probiotic 2 to 3 hours after your antibiotic dose. That gives the antibiotic time to do its job, then lets the probiotic settle in without being wiped out.
Some people take probiotics with food. Others take them on an empty stomach. It depends on the product. Acid-resistant strains like L. rhamnosus GG can handle stomach acid better, so they’re fine on an empty stomach. Others might need food to protect them. Check the label. If it doesn’t say, start with food - it’s safer.
Take them every day during your antibiotic course, and keep going for at least a week after you finish. Your gut needs time to rebuild.

What You Might Feel at First
When you start taking probiotics, your gut might react. Bloating. Gas. Mild cramping. That’s normal - especially if you’re not used to them. It’s not the probiotics being harmful. It’s your gut adjusting. These symptoms usually fade within a few days.
But if you feel worse - severe diarrhea, vomiting, fever - stop. That’s not adjustment. That’s a reaction. And if you’re immunocompromised, have a central line, or recently had surgery, talk to your doctor first. There have been rare cases of probiotics causing bloodstream infections in vulnerable people. It’s rare, but real.
The Big Problem: Unregulated Market
Here’s the scary part: in the U.S., probiotics are sold as dietary supplements. That means the FDA doesn’t test them for safety or effectiveness before they hit shelves. A 2022 ConsumerLab study found that 30% of probiotic supplements didn’t contain the number of live organisms they claimed. Fifteen percent had strains not listed on the label - including potentially harmful ones.
You’re buying a product that might be empty. Or worse, contaminated. That’s why brand matters. Look for companies that publish third-party lab results. Brands like Culturelle, Seed, and Renew Life often do. Avoid store brands with no transparency. If you can’t find a certificate of analysis on their website, don’t trust it.
And price? Doesn’t mean quality. Some expensive brands are just fancy packaging. Some cheap ones are solid. Check the strain. Check the CFU count. Check the expiration date. Probiotics die over time. If the bottle says “best by” but doesn’t guarantee live cultures at that date, skip it.
Who Should Avoid Probiotics?
Most healthy people can take them safely. But if you have:
- A weakened immune system (from cancer treatment, HIV, or organ transplant)
- Been recently hospitalized or had major surgery
- Are critically ill or on a ventilator
- Have a central IV line or artificial heart valve
- then talk to your doctor first. There are documented cases of probiotics causing serious infections in these groups. What’s safe for you might be dangerous for them.
What About Food Sources?
Yogurt, kefir, sauerkraut, kimchi - all have live cultures. But they’re not reliable for preventing antibiotic diarrhea. Why? The dose is too low. A serving of yogurt might have 1 billion CFUs. You need 10 billion to see benefit. And the strains? Often not the ones proven to help. Food is great for daily gut health. But during antibiotics, you need the power of a targeted supplement.
What’s Next for Probiotics?
Research is moving fast. The NIH just funded $12.5 million in new studies to figure out which probiotic strains work best with which antibiotics. Scientists are even looking at personalized probiotics - matching the right bug to your gut type and antibiotic regimen.
But until then, stick with what works: Saccharomyces boulardii or Lactobacillus rhamnosus GG, taken 2-3 hours after your antibiotic, daily for the full course plus one week. Don’t guess. Don’t buy random blends. Pick a trusted brand. Check the label. And if you’re unsure? Ask your doctor or pharmacist. They’ve seen what works - and what doesn’t.
Frequently Asked Questions
Can I take probiotics while on antibiotics for a urinary tract infection?
Yes. Antibiotics for UTIs, like nitrofurantoin or ciprofloxacin, still disrupt your gut microbiome, even if they’re targeting your bladder. Probiotics won’t interfere with the antibiotic’s action on the urinary tract, but they can help reduce the diarrhea and bloating that often come with these drugs. Stick to L. rhamnosus GG or S. boulardii, and take them 2-3 hours after your antibiotic.
Do probiotics make antibiotics less effective?
No, not when taken correctly. Probiotics don’t neutralize antibiotics. The key is timing. Taking them 2-3 hours apart ensures the antibiotic kills the bad bacteria without wiping out the good ones you’re trying to reintroduce. Studies show no reduction in antibiotic effectiveness when probiotics are used this way.
How long should I keep taking probiotics after finishing antibiotics?
Continue for at least one to two weeks after your last antibiotic dose. Your gut microbiome doesn’t bounce back overnight. Studies show that taking probiotics for this period reduces the chance of lingering diarrhea and helps your natural bacteria re-establish. Some people choose to keep taking them long-term for general gut health - that’s fine, as long as you’re using a quality product.
Can I get enough probiotics from yogurt instead of supplements?
Yogurt and fermented foods are healthy, but they’re not strong enough to prevent antibiotic-associated diarrhea. Most yogurts contain only 1-2 billion CFUs per serving, and the strains aren’t always the ones proven to help. For targeted protection during antibiotic therapy, you need a supplement with at least 10 billion CFUs of L. rhamnosus GG or S. boulardii.
Are there any side effects of taking probiotics with antibiotics?
Most people experience mild bloating or gas at first - this usually goes away in a few days. Rarely, people with weakened immune systems can develop infections from probiotics. If you feel worse - fever, severe cramping, bloody stool - stop taking them and contact your doctor immediately. Also, avoid probiotics if you’ve had recent surgery or have a central IV line.


12 Comments
Been on antibiotics twice this year and started taking Culturelle right away-no more stomach chaos. Seriously, life-changing. I didn’t believe it at first, but now I’m hooked.
Probiotics are a scam. My gut’s been fine without them. All this hype is just Big Yogurt pushing supplements. You don’t need magic bugs to recover from antibiotics.
Jim, I get where you’re coming from, but the Cochrane review is pretty solid-70% drop in C. diff risk with proven strains. It’s not about magic, it’s about science. I work in pharmacy and see people crash from antibiotic diarrhea all the time. Probiotics aren’t optional for high-risk folks.
I took a random probiotic from Walmart and got worse. Now I’m terrified of anything labeled ‘live cultures.’ Why can’t they just make these things reliable?
If you’re taking probiotics, you’re probably the kind of person who thinks kale fixes everything. Antibiotics are medicine. Your gut will fix itself if you stop meddling with it. Stop buying into wellness cult nonsense.
Hey Nicole, I get you’re skeptical-but I’ve seen too many grandma patients get hospitalized from C. diff after antibiotics. Probiotics aren’t a cure-all, but for the right people? They’re a shield. And yeah, some brands are trash, but the good ones? Totally worth it. Just pick L. rhamnosus GG or S. boulardii. Easy.
While I appreciate the comprehensive nature of this exposition, I must respectfully interject that the commercialization of probiotics in the United States remains an unregulated quagmire, wherein the consumer is often left to navigate a labyrinth of mislabeled, underpotent, and occasionally adulterated products under the guise of ‘wellness.’ One must exercise extreme diligence, as the absence of FDA pre-market approval renders the market a veritable Wild West of microbial marketing.
Hi, I am from India and take Saccharomyces boulardii with my antibiotics. Works great! I buy it from local pharmacy, but always check expiry date. Some brands here are fake, so be carefull.
For anyone new to this-start with Culturelle or Seed. Take it 2 hours after your antibiotic. Don’t skip the week after. Your gut will thank you. And if you’re worried about quality, just Google the brand + ‘third-party testing’-most legit ones show their lab results. No guesswork needed.
It’s hilarious how people treat probiotics like vitamins. You wouldn’t swallow random pills from a gas station and call it ‘medicine.’ Yet here we are, trusting a $12 bottle with no active ingredient verification. If you’re going to take something this important, at least pay for a brand that publishes its CFU counts and strain IDs. Otherwise, you’re just feeding your gut placebo.
Sharleen is right about the lack of regulation, but I’d add that even some ‘trusted’ brands fail batch testing. Always check the Certificate of Analysis on the manufacturer’s site. If it’s not there, assume nothing is guaranteed. Also, store probiotics in the fridge if possible-heat kills the bugs faster than you think.
My mom had C. diff after a hospital stay. She was in ICU for weeks. We started her on S. boulardii the moment she got home-she didn’t have one recurrence in 18 months. I don’t care what the skeptics say. This isn’t wellness fluff. It’s prevention. And if you’re on antibiotics, you owe it to yourself to do the one thing that actually reduces risk. Don’t be the person who says ‘I didn’t know.’ Now you do.