
When your doctor orders pulmonary function tests, they’re not just checking if you can breathe. They’re looking for hidden problems in your lungs-problems that might not show up on a chest X-ray or even make you cough. Two of the most important tests in this group are spirometry and DLCO. Together, they give a complete picture: one tells you how well air moves in and out of your lungs, the other tells you how well oxygen gets into your blood. Most people understand spirometry. Few understand DLCO. And that’s where things go wrong.
What Spirometry Actually Measures
Spirometry is simple. You take the deepest breath you can, then blow out as hard and fast as you can into a tube connected to a machine. The machine records two numbers: how much air you blew out in the first second (FEV1), and how much you blew out total (FVC). Then it calculates the ratio: FEV1 divided by FVC.
That ratio is the key. If it’s below 0.7, you have airflow obstruction. That’s asthma, COPD, or bronchitis. If it’s normal or high, but your total volume (FVC) is low, you might have restriction. But here’s the trap: restriction isn’t always what it looks like.
Some people with severe emphysema have low FVC-not because their lungs are stiff, but because they’re full of trapped air. Their lungs are big, but they can’t empty properly. That’s called pseudorestriction. Spirometry alone can’t tell the difference. That’s where DLCO comes in.
What DLCO Really Means
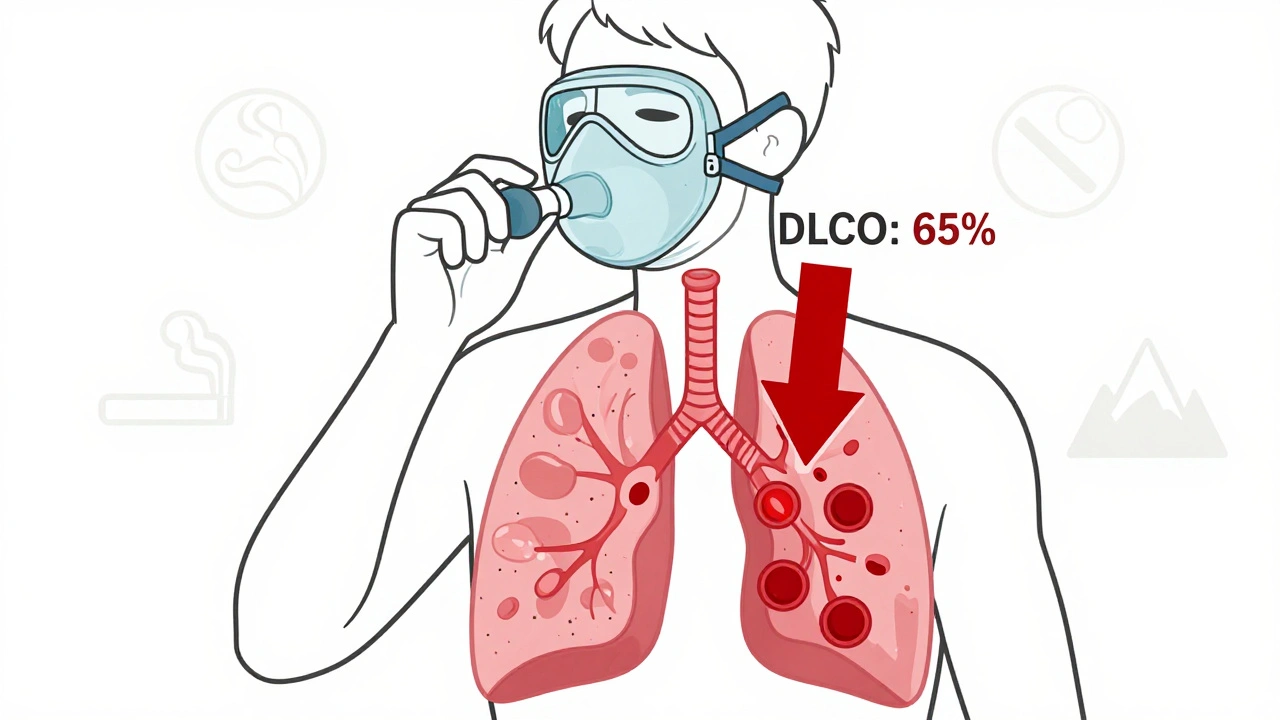
DLCO stands for diffusing capacity of the lung for carbon monoxide. It sounds technical, but it’s really just a measure of how well oxygen moves from your lungs into your bloodstream. You inhale a tiny, safe amount of carbon monoxide mixed with helium and oxygen. You hold your breath for 10 seconds. Then you exhale. The machine measures how much CO was absorbed.
Why carbon monoxide? Because it binds to hemoglobin 200 times more tightly than oxygen. So if your lungs can’t transfer CO well, they won’t transfer oxygen well either. Normal DLCO is between 75% and 140% of what’s predicted for your age, height, sex, and hemoglobin level. Below 75%? That’s a problem.
But here’s what most doctors miss: DLCO doesn’t just tell you if your lungs are damaged. It tells you where the damage is.
Why DLCO Beats Spirometry for Early Detection
People with interstitial lung disease-like pulmonary fibrosis-often have normal spirometry in the early stages. Their lungs still move air fine. But the walls between the air sacs are thickening. Oxygen can’t cross. DLCO drops first. Studies show it can fall to 60-70% of predicted 12 to 18 months before spirometry changes. That’s a huge window to catch something before it gets worse.
Same with early emphysema. You can have a perfectly normal FEV1/FVC ratio and still have destroyed alveoli. The air sacs are gone. The surface area for gas exchange is shrinking. DLCO will be low. Spirometry won’t catch it. That’s why some patients with unexplained shortness of breath, normal spirometry, and low DLCO end up getting a CT scan-and find early emphysema.
DLCO and the Big Three: Restriction, Obstruction, and Mixed
Let’s say your spirometry shows low FVC. Is it true restriction? Or just air trapping?
- If DLCO is low → it’s true restriction. Your lung tissue is stiff or scarred. Think pulmonary fibrosis, sarcoidosis, or asbestosis.
- If DLCO is normal or high → it’s extraparenchymal restriction. Your lungs are fine, but something’s squishing them. Think obesity, scoliosis, or a weak diaphragm.
Now look at obstruction. If you have COPD or asthma:
- DLCO is often low → that’s emphysema. The lung tissue is gone.
- DLCO is normal or high → that’s asthma. Your airways are inflamed, but your gas exchange surface is intact. In fact, during an asthma attack, DLCO can go up because of increased blood flow to the lungs.
And then there’s the FVC/DLCO ratio. If this number is above 1.6, you have a high chance of pulmonary hypertension. That’s because your lung blood vessels are narrowed or blocked. Your lungs are trying to pump blood through a shrinking pipeline. The body compensates by increasing pressure. DLCO drops. FVC stays normal. The ratio spikes.
What Makes DLCO Go Wrong (Besides Lung Disease)
DLCO is sensitive. Too sensitive. A few things can make it look abnormal when your lungs are fine.
- Anemia: Every 1 g/dL drop in hemoglobin lowers DLCO by about 1%. If your blood count is low, your DLCO will be too-no lung damage needed.
- Smoking: Carbon monoxide from cigarettes sticks to your hemoglobin. That leaves less room for the test gas. DLCO drops by 5-10%. Always ask if the patient smoked in the last 24 hours.
- High altitude: Less oxygen in the air means less driving force for gas exchange. DLCO can be falsely low.
- Not holding your breath long enough: The test requires exactly 10 seconds. If you exhale too soon, the result is invalid.
That’s why every DLCO test needs a hemoglobin level. Without it, you’re guessing. And guessing with DLCO can lead to misdiagnosis.
When DLCO Is High-And Why That Matters
High DLCO isn’t common, but it’s telling. If your DLCO is above 140%, you might have:
- Asthma during an attack
- Pulmonary hemorrhage (blood leaking into the air sacs)
- Polycthemia (too many red blood cells)
- A heart defect with a left-to-right shunt (blood bypassing the lungs)
These aren’t trivial findings. A high DLCO in someone with shortness of breath could mean internal bleeding in the lungs-or a congenital heart problem. It’s not something you ignore.
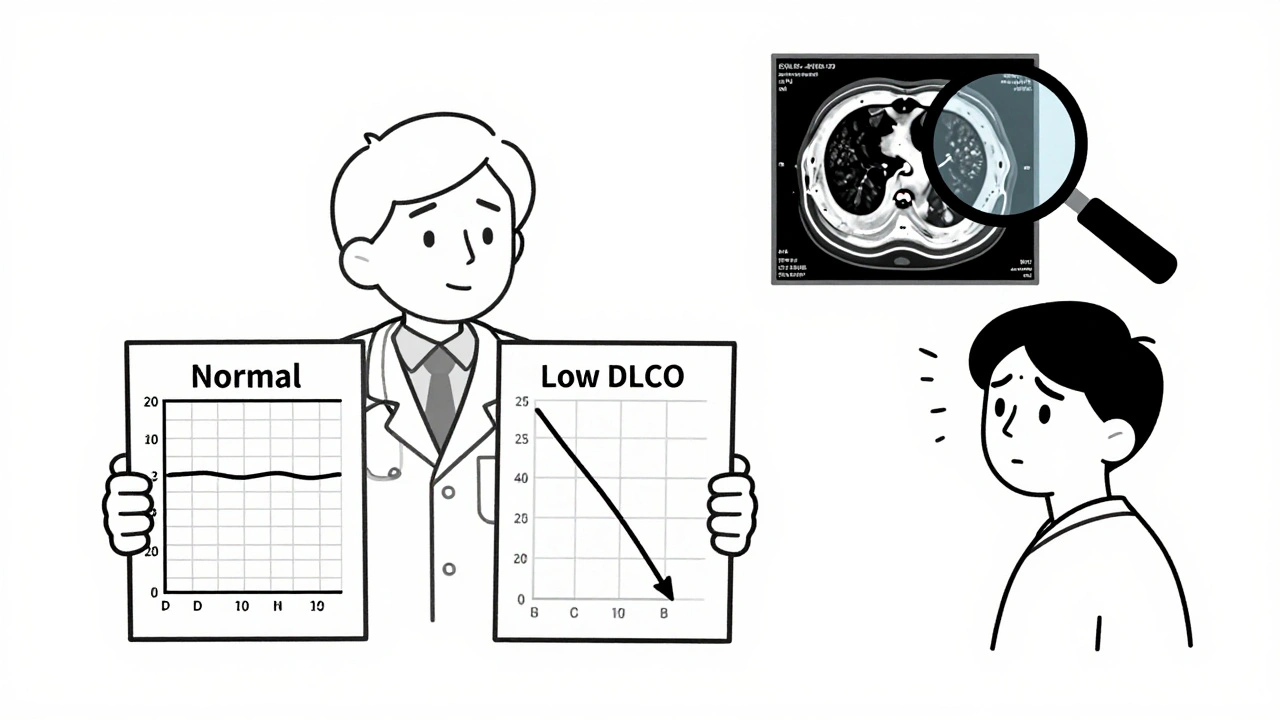
How Doctors Use These Tests Together
Here’s the real-world flow:
- Do spirometry first. If FEV1/FVC is below 0.7 → obstruction. Treat accordingly.
- If FEV1/FVC is normal but FVC is low → suspect restriction. Now check DLCO.
- If DLCO is low → investigate interstitial lung disease, pulmonary vascular disease, or emphysema.
- If DLCO is normal → look for mechanical causes: obesity, chest wall deformity, neuromuscular disease.
- If spirometry is normal but you still have symptoms → check DLCO. If it’s low, you need a CT scan or further workup.
That last step is critical. Many patients are told, “Your lungs are fine,” because their spirometry looks normal. But if their DLCO is 65%, their lungs are not fine. They just haven’t lost airflow yet.
What’s New in 2025
DLCO isn’t just a diagnostic tool anymore. It’s a prognostic one. In pulmonary fibrosis, a DLCO below 35% of predicted means a nearly threefold higher risk of death within two years. That’s why it’s now a required measurement in clinical trials for new drugs.
AI tools are starting to help. A 2023 Mayo Clinic study showed algorithms could predict pulmonary hypertension from DLCO patterns with 88% accuracy-better than many doctors. These tools aren’t replacing clinicians. They’re helping them spot patterns they might miss.
Reimbursement hasn’t changed much. Spirometry still costs about $50. DLCO is closer to $100. But usage is rising. More clinics are doing both tests routinely for unexplained shortness of breath. And that’s good.
What You Should Ask Your Doctor
If you’ve had these tests:
- Did you get both spirometry and DLCO?
- Was my hemoglobin checked before the DLCO?
- What’s my FEV1/FVC ratio? Is it below 0.7?
- What’s my DLCO as a percentage of predicted? Is it below 75%?
- Does my result suggest lung tissue damage, blood vessel problems, or something else?
Don’t let normal spirometry fool you. If you’re still short of breath, ask for DLCO. It’s the test that finds what spirometry can’t.
Can spirometry detect pulmonary fibrosis?
Spirometry often appears normal in early pulmonary fibrosis. It measures airflow, not gas exchange. By the time FVC drops, the disease is already advanced. DLCO is the first test to show abnormalities-sometimes 12 to 18 months earlier. That’s why DLCO is essential for early detection.
Why is DLCO low in emphysema?
Emphysema destroys the walls between air sacs, reducing the surface area where oxygen and carbon monoxide can transfer into the blood. Even if air moves in and out normally (normal spirometry), the lungs can’t exchange gases efficiently. That’s why DLCO drops, often before FEV1 does.
Does smoking affect DLCO results?
Yes. Smoking raises carboxyhemoglobin levels in your blood. This blocks the carbon monoxide used in the test from binding properly, making DLCO appear lower than it really is. Always avoid smoking for at least 24 hours before the test.
Can I have normal DLCO and still have asthma?
Yes. Asthma primarily affects the airways, not the gas exchange surface. DLCO is usually normal or even elevated during an attack because of increased lung blood flow. Normal DLCO doesn’t rule out asthma-it just means the problem isn’t in the lung tissue.
What if my DLCO is low but my spirometry is normal?
This is a red flag. It suggests early interstitial lung disease, pulmonary vascular disease, or anemia. You need further evaluation-likely a chest CT scan and blood work, including hemoglobin and iron levels. Don’t dismiss it just because you can breathe out fine.
Is DLCO testing painful?
No. It’s completely non-invasive. You breathe in a harmless gas mixture, hold your breath for 10 seconds, then breathe out. Some people feel dizzy or lightheaded briefly, but serious side effects are extremely rare. The only discomfort is holding your breath, which can be hard if you’re very short of breath.




15 Comments
DLCO is such an underused tool-so many patients get told 'your lungs are fine' when their DLCO is in the 60s. I’ve seen it too many times. Always check hemoglobin too. One time, a patient had a low DLCO, turned out they were anemic from heavy periods. No lung disease at all. Just low iron. 😊
Why do we even bother with DLCO when spirometry is cheaper and everyone already knows what it means I mean come on
The physiological rationale underpinning DLCO as a surrogate marker for alveolar-capillary membrane integrity is fundamentally sound, yet its clinical adoption remains suboptimal due to systemic underinvestment in pulmonary diagnostics. The confounding variables-hemoglobin saturation, COHb, altitude-demand rigorous standardization protocols that are rarely implemented in primary care settings.
This is such a clear breakdown. I work in a pulmonology clinic and we’ve started pushing DLCO for anyone with unexplained dyspnea-even if spirometry is normal. One patient had a DLCO of 58%, normal FEV1/FVC. Turned out it was early sarcoidosis. We caught it before fibrosis set in. Always pair it with hemoglobin. And yes, smoking the day before? Totally skews it. Thanks for laying this out.
DLCO is the unsung hero of lung tests. If you're breathless but your spirometry looks good? Ask for it. No excuses.
But... isn't this all just... Western medicine dogma? What about Qi? Or Ayurvedic prana? We're reducing the soul of breath to a number. Carbon monoxide? Really? We're poisoning ourselves to diagnose ourselves. There's a metaphysical truth here that science refuses to see...
Great summary. I’d add one thing: DLCO normalization after treatment can be a powerful indicator of response-especially in vasculitis or early IPF. Also, remember that DLCO can be falsely elevated in asthma during exacerbations due to increased pulmonary perfusion. Don’t assume normal = no asthma. It’s a dynamic test. And yes, always check hemoglobin. I’ve seen so many patients get mislabeled as having interstitial disease because their Hb was 9.2. Fix the anemia, retest. Magic.
Why do doctors even bother with this? It’s so expensive. And what about people who don’t smoke or have no family history? Why are we pathologizing normal breathing? My cousin’s grandma had low DLCO and they gave her a CT scan, turns out she just lives at 5,000 ft. And now she’s terrified of flying. This is medical overreach. 😔
This is super helpful. I’ve had shortness of breath for years and my doctor always said my lungs were fine. I asked for DLCO last month-my number was 68%. We found a small clot in my lungs. I wish I’d known about this sooner. Don’t wait until you’re gasping. Ask for the test. It’s not scary. Just breathe in, hold, breathe out. That’s it.
STOP letting doctors skip DLCO!! I’ve been breathless for 3 years. 3 YEARS. They said 'your lungs are fine' because spirometry looked good. Then I found this article. Got the DLCO done. 62%. Turned out early pulmonary hypertension. I’m on meds now and breathing again. If you’re tired and your doctor says 'it’s all in your head'-GET THE DLCO. You deserve to breathe.
DLCO is basically the lung’s version of a lie detector test. You think you’re fine? Ha. The CO laughs at your spirometry. It knows. It knows when your alveoli are turning to dust. It knows when your blood’s too thin. It knows when you smoked a cigarette this morning. And it doesn’t care how much you paid for your fancy gym membership. Your lungs are lying. The machine isn’t.
It’s fascinating how this test, so clinically valuable, is still treated as a second-tier diagnostic tool. The reimbursement disparity is grotesque-$50 for spirometry, $100 for DLCO-yet the latter provides exponentially more diagnostic insight. The system incentivizes ignorance. Clinicians default to the cheaper test because the payer won’t cover the nuanced one. This isn’t medicine-it’s actuarial theater.
I just wanted to say thank you for explaining this so clearly. I read this after my DLCO came back low and I was confused. Now I get why my doctor ordered a CT. I forgot to mention I was anemic-my Hb was 10.1. So the DLCO was low for that reason. I’m getting iron now. So glad I didn’t panic. 😊
In India we rarely do DLCO because cost and infrastructure. But your explanation is very good. We should train more doctors. Also smoking is big problem here. Many patients smoke before test. Result wrong. Need awareness.
Love that you mentioned the FVC/DLCO ratio. I just saw a case last week-normal FVC, DLCO at 55%, ratio over 1.8. Patient had no symptoms. CT showed mild pulmonary hypertension. We started them on anticoagulants and referral to pulm hypertension clinic. That ratio is a silent alarm. Most docs miss it.