
When your nose runs nonstop in spring, or you’re constantly stuffed up all year long, it’s not just a cold-it’s allergic rhinitis. This isn’t a minor nuisance. It’s an immune system overreaction to everyday things like pollen, dust mites, or pet dander. Millions of people deal with sneezing, itchy eyes, and blocked noses every day, and most of them aren’t treating it right.
What’s the Difference Between Seasonal and Perennial Allergic Rhinitis?
Seasonal allergic rhinitis hits during specific times of the year-usually spring, summer, or early fall-when plants release pollen. Tree pollen shows up in March and April, grasses peak in late spring and early summer, and weeds like ragweed dominate in late summer and early fall. If your symptoms match the calendar, you’re likely dealing with seasonal triggers.
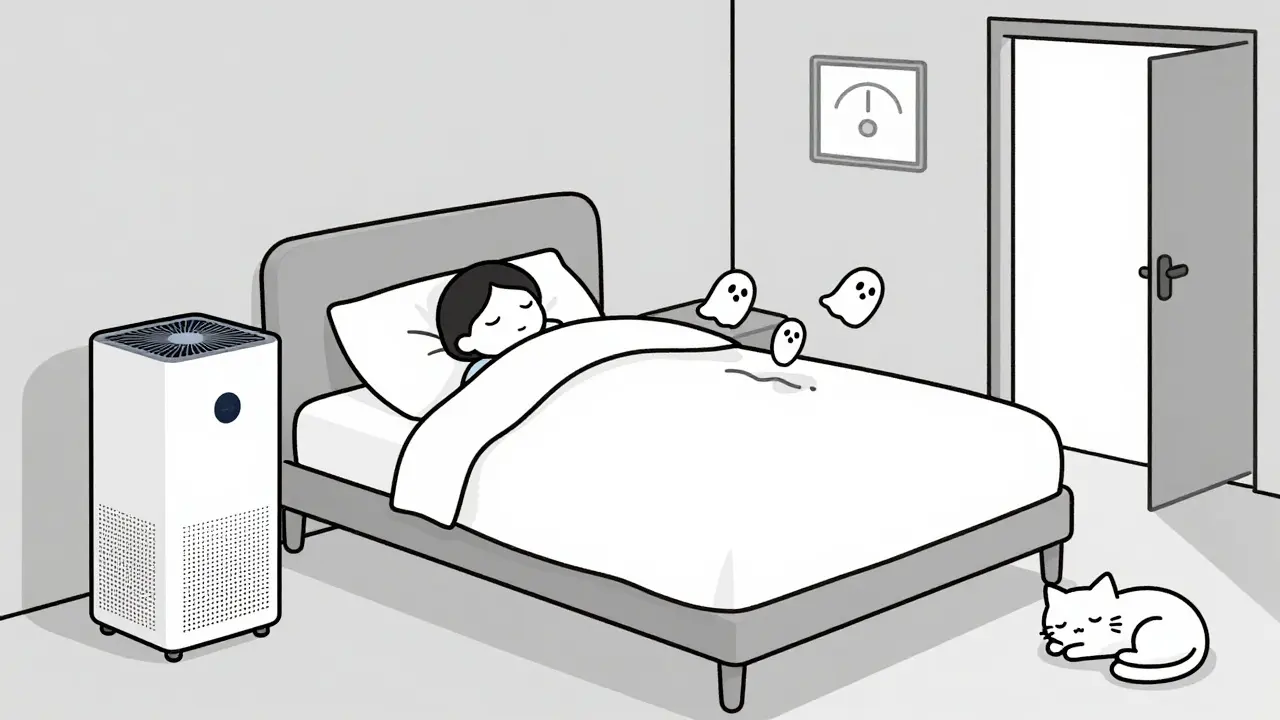
Perennial allergic rhinitis, on the other hand, never takes a break. It’s caused by indoor allergens that are always around: dust mites in your mattress, pet dander from your cat or dog, mold in damp bathrooms, or even cockroach particles in older homes. These allergens don’t vanish with the seasons, so your symptoms stick around year-round.
The key difference? Timing. Seasonal = weather-dependent. Perennial = home-dependent. But both trigger the same reaction: your body releases histamine, causing swelling, mucus, and itching in your nasal passages.
First-Line Treatment: Intranasal Corticosteroids
If you’ve got moderate to severe symptoms-especially nasal congestion-intranasal corticosteroids are your best bet. These aren’t the same as the steroids athletes abuse. These are tiny, targeted sprays that reduce inflammation right where it’s happening: inside your nose.
Common options include fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort). They’re available over the counter now, but they don’t work overnight. You need to use them every day for at least a week before you feel real relief. That’s why so many people quit too soon.
Here’s the catch: 60-70% of people use these sprays wrong. They aim straight up the middle of the nose, which irritates the sensitive septum and can cause nosebleeds. The right way? Tilt your head slightly forward, point the spray toward the outer wall of your nostril (not the middle), breathe in gently, and don’t blow your nose for 15 minutes after. Do it right, and you’ll cut symptoms by 30-50%.
Oral Antihistamines: Fast Relief for Itching and Sneezing
If your main issues are sneezing, itchy nose, or watery eyes, oral antihistamines like cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra) work fast-within an hour. These are second-generation drugs, so they don’t make most people drowsy. First-gen ones like diphenhydramine (Benadryl) do, but they’re not recommended for daily use because they’re less effective long-term and can mess with your sleep and focus.
But here’s the truth: antihistamines barely touch nasal congestion. If you’re stuffed up, they won’t fix it. That’s why many people take them and still feel miserable. They’re great for itching and sneezing, but not for breathing. Use them as a sidekick to your nasal spray, not the main weapon.
Decongestants: Use With Caution
When your nose is completely blocked, you might reach for pseudoephedrine (Sudafed) or oxymetazoline spray (Afrin). They work fast. But they’re like a fire alarm-useful in an emergency, dangerous if you keep pulling the handle.
Oral decongestants can raise your blood pressure, cause jitteriness, and interfere with sleep. Don’t use them longer than 3-7 days. Nasal sprays? Even riskier. Using oxymetazoline for more than three days in a row can lead to rebound congestion-your nose gets worse when you stop. It’s called rhinitis medicamentosa. You end up needing more spray just to feel normal. That’s a trap.
Immunotherapy: The Only Treatment That Changes the Course
Medications manage symptoms. Immunotherapy changes your immune system’s response. That’s why it’s the only treatment that can potentially stop allergies from getting worse over time.
There are two types: allergy shots (subcutaneous immunotherapy, or SCIT) and allergy tablets (sublingual immunotherapy, or SLIT). Shots are given weekly at first, then monthly, over 3-5 years. They’re slightly more effective-cutting symptoms by 35-45%-but require clinic visits and carry a small risk of anaphylaxis (0.2% per shot).
SLIT tablets, like Oralair or Grastek, are taken under the tongue daily. They’re easier. You can do them at home after the first dose (which must be done in a doctor’s office). But they only work for specific allergens: grass, ragweed, or dust mites. And they come with side effects-most people get mild mouth itching, and 32% quit within the first year because of it.
Both options require commitment. You won’t feel better for months. But if you stick with it, you might reduce your need for meds long-term. The American Academy of Allergy, Asthma & Immunology recommends considering immunotherapy if your symptoms are severe, meds aren’t helping, or you can’t avoid your triggers.
Environmental Control: Reduce Exposure at Home
Medications help, but if you’re still breathing in allergens, you’re fighting a losing battle. You need to clean up your environment.
For dust mites: Wash bedding weekly in water hotter than 130°F (54°C). Use allergen-proof covers on your mattress and pillows. These reduce exposure by 83%. Keep indoor humidity below 50% with a dehumidifier-dust mites die in dry air.
For pet dander: Keep pets out of the bedroom. Use a HEPA air purifier in your main living area. Vacuum weekly with a HEPA-filter vacuum. Bathe pets every 1-2 weeks.
For mold: Fix leaks. Clean bathroom grout with vinegar. Use exhaust fans. Don’t let damp towels sit around.
For pollen: Check daily pollen counts (apps like Pollen Sense are reliable). Keep windows closed when counts are above 9.7 grains per cubic meter. Wear wraparound sunglasses outside-this cuts eye symptoms by 35%. Shower and change clothes after being outdoors during high-pollen days.
What About Saline Rinses?
Nasal saline irrigation isn’t a cure, but it’s a powerful helper. Rinsing your nose with saltwater flushes out allergens, mucus, and irritants. A 2022 survey found 62% of users felt better when they did it twice daily alongside their meds.
Use a neti pot or squeeze bottle with distilled or boiled (then cooled) water. Don’t use tap water-it can carry dangerous microbes. Start with a gentle stream. Some people feel weird at first, but most adapt quickly.

Emerging Treatments and What’s Next
In October 2023, the FDA approved tezepelumab, the first biologic for allergic rhinitis. It targets a protein called TSLP that kicks off the allergic cascade. Early results show a 42% reduction in symptoms. It’s still new, expensive, and for severe cases only.
There’s also a new combo spray: azelastine (an antihistamine) with fluticasone (a steroid). It works faster than steroid sprays alone-relief in 30 minutes-and reduces congestion better than either drug alone. It’s prescription-only, but it’s changing how doctors treat moderate-to-severe cases.
By 2030, personalized allergy testing-looking at specific proteins in allergens, not just whole pollen or dust mite extracts-will guide treatment. This means you’ll get therapies tailored to your exact immune response, not a one-size-fits-all approach.
Why Most People Don’t Get Better
Here’s the uncomfortable truth: 60% of people with allergic rhinitis start with OTC antihistamines and wait 3.2 years before seeing a specialist. By then, their symptoms are chronic, their quality of life is down, and their sleep and focus are shot.
Why? Because they think it’s just “bad allergies” and not a real medical condition. Because they don’t know how to use nasal sprays. Because they expect instant results from steroids and give up. Because they don’t realize that avoiding allergens is part of the treatment.
Improvement isn’t about trying more drugs. It’s about using the right ones, the right way, and combining them with real environmental changes. If you’re still struggling after months of antihistamines, it’s not your fault-it’s your plan.
What to Do Next
Step 1: Track your symptoms. When do they happen? What makes them worse? Keep a simple log for two weeks.
Step 2: If you’re congested, start a nasal corticosteroid spray. Use it daily for at least 10 days. Learn the correct technique.
Step 3: If itching and sneezing are worse, add a non-drowsy antihistamine. Don’t double up on decongestants.
Step 4: Clean your bedroom. Wash bedding. Use pillow covers. Lower humidity.
Step 5: If you’re still not better after 6-8 weeks, see an allergist. Ask about allergy testing and immunotherapy. Don’t wait another year.
Allergic rhinitis doesn’t have to control your life. With the right strategy, you can breathe easier, sleep better, and stop feeling like you’re always fighting a cold.
Can allergic rhinitis turn into asthma?
Yes. People with allergic rhinitis are more likely to develop asthma, especially if it’s untreated. Studies show that kids with allergic rhinitis who get immunotherapy for three years cut their risk of developing asthma by 67%. The inflammation in your nose doesn’t stay there-it can spread to your lungs. Treating rhinitis early helps protect your airways.
Are nasal corticosteroids safe for long-term use?
Yes. At recommended doses, intranasal corticosteroids have minimal absorption into the bloodstream. Studies over 10+ years show no significant impact on bone density, growth in children, or adrenal function. Side effects like nosebleeds or dryness are local and rare. The risk of not treating moderate-to-severe symptoms-like poor sleep, missed work, or worsening asthma-is far greater.
Why do my allergies get worse at night?
Nighttime symptoms are usually caused by indoor allergens. Dust mites thrive in your bedding, and pet dander collects on pillows. Lying down also lets mucus pool in your nose, making congestion worse. Use allergen-proof covers, wash sheets weekly in hot water, and keep pets out of the bedroom. A HEPA air purifier near your bed can also help.
Can I outgrow allergic rhinitis?
Some people do, especially children. About 20-30% of kids with allergic rhinitis see significant improvement by their late teens. But for adults, it’s rare to outgrow it completely. Symptoms can change with environment or immune system shifts, but without treatment, they usually persist. Immunotherapy offers the best chance at long-term reduction.
Is there a natural cure for allergic rhinitis?
No. Supplements like quercetin, butterbur, or probiotics have been studied, but none show consistent, strong evidence in large trials. Some people report feeling better with honey or acupuncture, but these aren’t backed by science. The only proven methods are allergen avoidance, FDA-approved medications, and immunotherapy. Don’t waste money on unproven remedies-focus on what actually works.



