When the FDA releases a safety alert about a medication, it’s easy to panic. You see headlines like "FDA warns of heart risk with common diabetes drug" and immediately wonder: Should I stop taking it? Is this dangerous? The truth is, most of these alerts don’t mean you need to stop your medicine - but they do mean you need to understand what’s really being said. The FDA doesn’t issue these warnings lightly, but they’re not final verdicts either. They’re signals. And learning how to read them correctly can keep you safe without causing unnecessary fear.
What the FDA Actually Means by "Potential Signal"
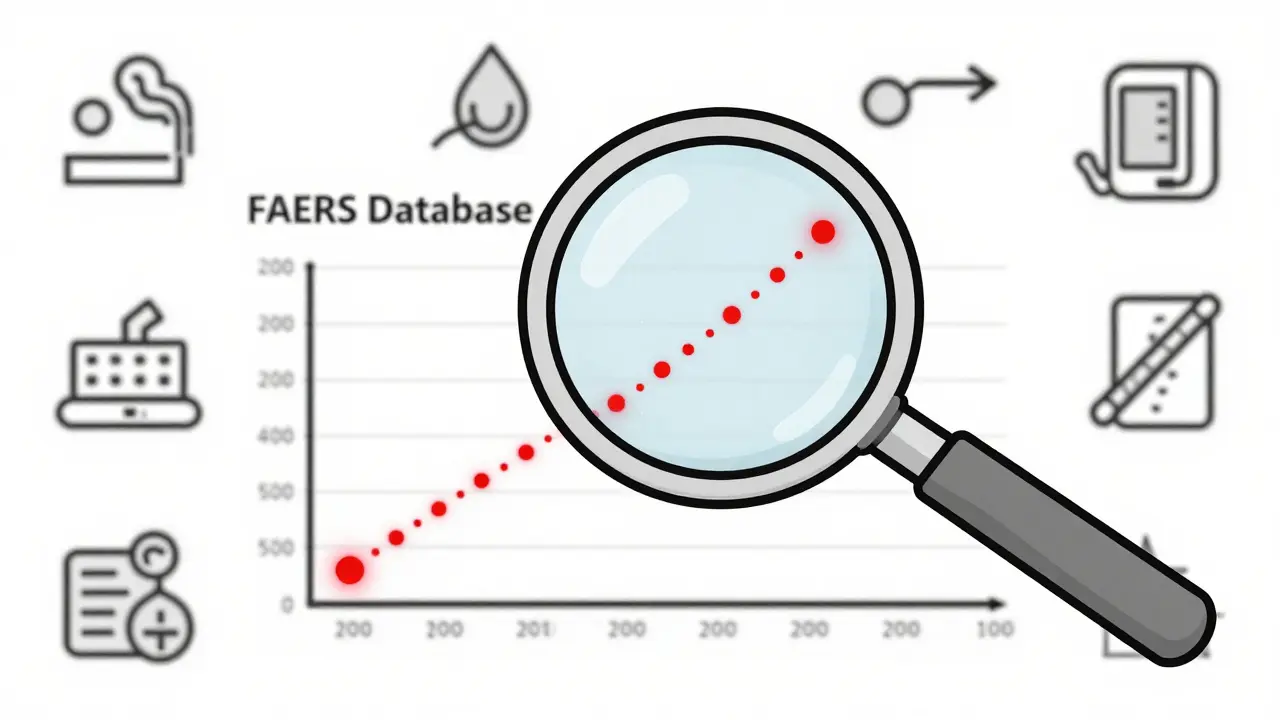
Many FDA safety announcements start with the phrase "potential signal." That’s not a red flag - it’s a yellow one. A potential signal means the FDA has noticed something unusual in its data. Maybe more people taking Drug X reported kidney problems than expected. But that doesn’t mean Drug X caused those problems. It just means they’re looking closer. The FDA collects over 25 million adverse event reports in its FAERS database. Most of these are incomplete. A patient might report "chest pain" after taking a pill, but they also have high blood pressure, smoke, and haven’t exercised in years. The FDA can’t tell from that single report whether the drug was to blame. So they look at patterns across thousands of reports. If a certain side effect shows up significantly more often in users of a drug than in non-users, that’s when they flag it as a potential signal. Here’s the key: The FDA says clearly in every alert that "this does not mean FDA has determined that the drug has the risk". If you see an alert and immediately stop your medication, you might be trading one risk for another - especially if your condition is serious and the drug is helping.Understanding the Difference Between Adverse Events and Adverse Reactions
Not every bad thing that happens after taking a drug is the drug’s fault. The FDA makes a clear distinction:- Adverse Event (AE): Any negative medical occurrence that happens after taking a drug - whether or not the drug caused it.
- Adverse Drug Reaction (ADR): A harmful effect that is reasonably linked to the drug’s pharmacological action.
How to Read an FDA Drug Safety Communication
Most FDA safety alerts follow a predictable pattern. Here’s how to break them down:- Check the language: Is it "potential signal," "possible association," or "confirmed risk"? "Confirmed risk" means the FDA has strong evidence the drug causes the problem. "Potential signal" means they’re still studying it.
- Look for numbers: The best alerts give you context. For example, the August 2022 alert on SGLT2 inhibitors said: "Fournier’s gangrene occurred in 0.2 cases per 1,000 patient-years vs. 0.06 in non-users." That’s a 3-fold increase - but still extremely rare. If no numbers are given, the alert is vague and hard to act on.
- Ask: Is this risk serious?" The FDA defines "serious" as fatal, life-threatening, disabling, or requiring hospitalization. If the risk is mild - like a headache or nausea - it’s unlikely to change your treatment.
- Consider your condition: A 5% risk of liver injury might be too high for a mild acne drug - but acceptable for a cancer drug that extends life by months.
- Check if alternatives exist: If there’s no other drug that works as well, the benefit often outweighs the risk.
A 2022 AMA survey found that 42% of doctors changed prescriptions based on FDA alerts - only to later learn the risk was minimal. That’s why context matters more than the alert itself.
Why Some Alerts Cause More Confusion Than Clarity
In 2021, the FDA issued a safety alert linking COVID-19 vaccines to menstrual changes. Thousands of women called their doctors in panic. The alert was based on a few hundred anecdotal reports. There was no statistical evidence of increased risk. The FDA later clarified that the changes were likely due to stress, illness, or immune response - not the vaccine itself. This happens because the FDA has to act quickly. They can’t wait for perfect data. If they wait too long, people could get hurt. But their urgency sometimes creates public alarm. The agency admits this. In its 2024-2026 strategic plan, it’s committing to using standardized quantitative formats by 2025. That means future alerts will say things like: "This risk affects 1 in 5,000 users - compared to 1 in 10,000 in the general population."What You Should Do When You See an Alert
Don’t panic. Don’t stop your medicine. Do this instead:- Don’t act alone: Talk to your doctor or pharmacist. They know your history and can weigh the real risk for you.
- Check the date: Is this a new alert? Or did it come out two years ago and you just saw it? The FDA updates its website regularly. Some alerts are later withdrawn or clarified.
- Use the FDA’s Drug Safety Triaging Tool: Available online, this free tool helps clinicians and patients quickly categorize alerts by urgency and evidence strength. It cuts interpretation time by 35%.
- Report your experience: If you notice a new side effect, report it to MedWatch. The more data the FDA gets, the better its assessments become.
Remember: The goal of these alerts isn’t to scare you. It’s to give you and your doctor better information. The FDA’s system isn’t perfect - but it’s the most comprehensive drug safety monitoring system in the world. It has prevented thousands of avoidable deaths by catching risks like liver damage from acetaminophen, heart valve issues with fenfluramine, and birth defects from thalidomide long before they became widespread.
How the FDA Compares to Other Regulators
The European Medicines Agency (EMA) requires companies to submit a Periodic Benefit-Risk Evaluation Report (PBRER) every 6-12 months. Japan’s PMDA uses real-world data earlier in the approval process. But the FDA is unique in its quarterly public release of potential safety signals. This transparency is a strength - but also a weakness. It puts pressure on the agency to communicate uncertainty clearly. The FDA doesn’t have the same legal authority as the EMA to force label changes immediately. Instead, it works with manufacturers. If the FDA identifies a confirmed risk, it sends a Safety Labeling Change (SLC) letter. The company has 30 days to propose changes or argue against them. This process can take months. That’s why you sometimes see delays between an alert and updated labeling.
What’s Changing in 2025 and Beyond
The FDA’s new 2024-2026 plan includes three major improvements:- Standardized risk numbers: All future alerts will include clear, comparable rates - like "1 in 1,000" instead of "rare" or "uncommon."
- Condition-specific templates: Alerts for cancer drugs will look different than those for antidepressants, because the risk-benefit balance is completely different.
- Patient-facing tools: By 2026, the FDA will launch a website tool that lets patients visualize their personal risk based on age, gender, and other conditions.
These changes are coming because patients and doctors are demanding better information. A 2022 FDA survey found that 75% of patients who read safety alerts felt confused about whether to keep taking their medicine. That’s unacceptable. The goal now isn’t just to detect risks - it’s to communicate them in a way people can understand.
Final Takeaway: Trust the Process, Not the Headline
The FDA’s job isn’t to make drugs 100% safe - it’s to make sure the benefits outweigh the risks. Every approved drug carries some risk. Even aspirin can cause bleeding. But for millions, that risk is worth it. When you see an FDA safety announcement, ask yourself: Is this a confirmed risk? Is it serious? Do I have alternatives? Does this apply to me? If you’re unsure, talk to your provider. Don’t guess. Don’t stop. Just pause - and ask.Are FDA safety alerts a sign that I should stop taking my medication?
No, not automatically. FDA alerts often report "potential signals," which are early warning signs that require more study. Stopping medication without medical advice can be dangerous, especially for chronic conditions like high blood pressure, diabetes, or depression. Always consult your doctor before making changes.
What’s the difference between an adverse event and an adverse drug reaction?
An adverse event is any negative medical occurrence that happens after taking a drug - whether or not the drug caused it. An adverse drug reaction is a harmful effect that is reasonably linked to the drug’s pharmacological action. For example, a headache after taking a new pill is an adverse event. If the headache only happens with that specific drug and not others, it may be classified as an adverse drug reaction.
Why do some FDA alerts seem vague or confusing?
Many FDA alerts are based on incomplete data from voluntary reports. Without clear numbers or context, it’s hard to judge the real risk. The FDA is working to fix this by requiring standardized risk estimates in all future alerts by 2025. Until then, always seek clarification from a healthcare provider.
How does the FDA decide if a risk is "serious"?
The FDA defines a "serious" risk as one that is fatal, life-threatening, permanently disabling, or requires hospitalization. Mild side effects like nausea or dizziness are not considered serious, even if they’re unpleasant. The seriousness of the risk helps determine how urgently the FDA acts.
Can I trust FDA safety communications if they’re not always accurate?
Yes - but with context. The FDA’s system is designed to catch risks early, even if the evidence isn’t perfect. Many alerts are later refined or withdrawn after more data is collected. This is a feature, not a flaw. It means the system is working. The key is to use alerts as a starting point for discussion with your doctor - not as a final decision.
What to Do Next
If you’ve received an FDA safety alert about your medication:- Don’t stop taking it.
- Find the official FDA Drug Safety Communication on fda.gov.
- Look for numbers - how many people are affected?
- Check if the risk applies to your condition, age, or other medications.
- Call your doctor or pharmacist. Bring the alert with you.
Most people don’t need to change anything. But if you’re unsure, getting expert advice is always the right move. The FDA’s system works best when patients and providers work together - not when fear drives decisions.