If you’ve been getting headaches almost every day for months - not the sharp, throbbing kind, but a constant, dull pressure like a tight band around your head - you’re not alone. About 2-3% of adults worldwide live with chronic tension headaches (CTH), and most of them spent years being told it’s just stress. But this isn’t just ‘tension’ in the way people think. It’s not your neck muscles screaming for a massage. It’s your brain’s pain system gone haywire.
What Exactly Is a Chronic Tension Headache?
Chronic tension headache isn’t just frequent headaches. It’s defined by strict medical rules: at least 15 headache days a month for three months or more. And on at least eight of those days, the pain must match the classic pattern: a steady, non-throbbing ache on both sides of your head, not worse with movement, and no nausea or vomiting. You might feel sensitivity to light or sound, but not the intense, blinding kind that comes with migraines.
Unlike migraines, CTH doesn’t show up on scans. There’s no tumor, no aneurysm, no structural problem. Your MRI or CT scan will look normal. That’s why so many people are misdiagnosed. In fact, nearly 4 in 10 people with chronic daily headaches are wrongly labeled as having chronic migraine. The real clue? If you’re getting headaches every day and you’re not sensitive to light or sound most of the time, it’s likely CTH.
Why Your Muscles Aren’t the Real Culprit
You’ve probably heard that tension headaches are caused by tight muscles in your neck and scalp. That’s what most websites still say. But that’s outdated. A 2023 review of over 150 studies found that 78% of headache specialists now agree: muscle tightness is a side effect, not the cause.
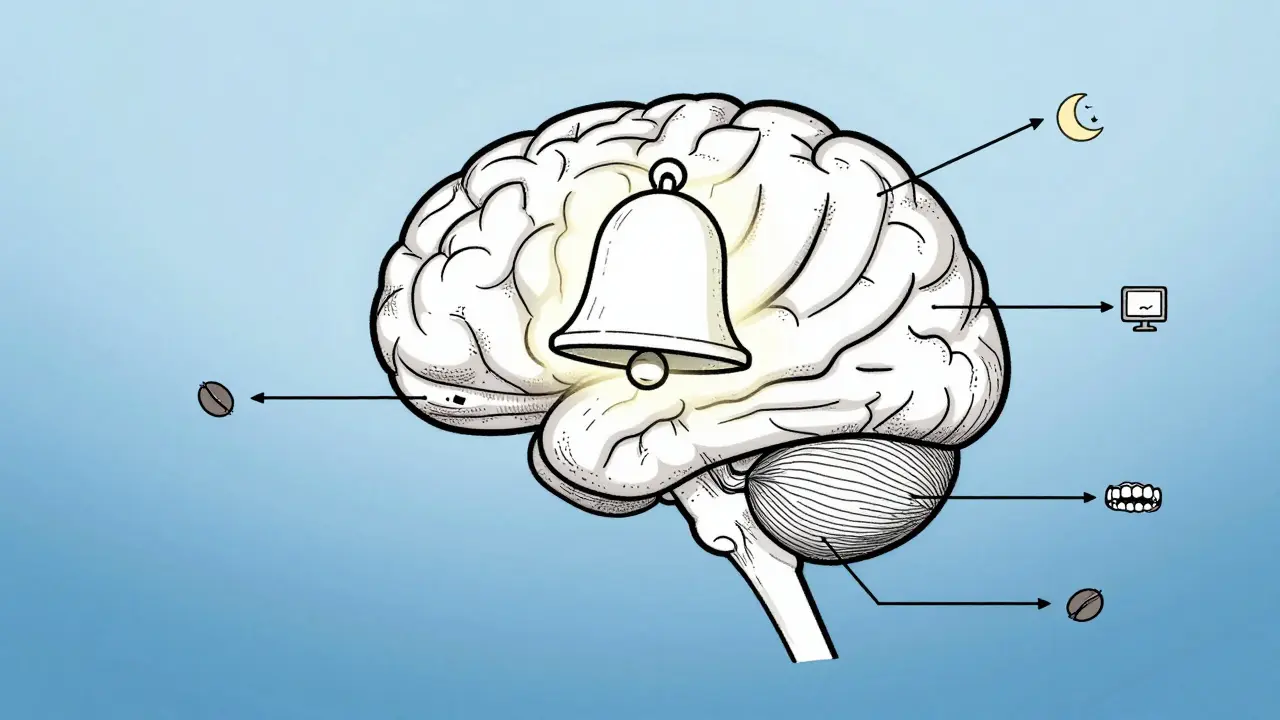
The real problem? Your brain’s pain system has become oversensitive. Think of it like a faulty alarm. In people with CTH, the nerves in your brainstem - especially the trigeminal nucleus caudalis - are stuck on high alert. Even normal signals from your neck or jaw get interpreted as pain. That’s why pressing on your temples or the back of your neck hurts - your brain is amplifying every tiny sensation.
This explains why massaging your neck helps temporarily - it distracts your brain. But it doesn’t fix the root issue. The same thing happens with stress. Stress doesn’t make your muscles clench so hard it causes a headache. Instead, stress raises your body’s cortisol levels by up to 37%, which lowers your pain threshold. Your brain becomes more likely to turn normal sensations into headaches.
What Actually Triggers These Headaches?
Triggers aren’t random. They’re measurable, and they’re often hidden in daily habits.
- Sleep disruption: Getting less than six hours a night makes you 4.2 times more likely to have a headache the next day.
- Caffeine swings: If you drink more than 200mg of caffeine daily (about two large coffees) and then skip your usual cup, withdrawal kicks in within hours - and so does the headache.
- Screen time: Looking at screens more than seven hours a day increases your risk by 63%. It’s not the blue light - it’s the staring. When you focus on a screen, you blink less, your eyes strain, and your jaw tenses. That’s why the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds) is one of the most effective prevention tools - endorsed by 83% of users in a recent survey.
- Jaw clenching: Even if you don’t grind your teeth at night, holding your jaw tight during work or while stressed can trigger headaches. EMG studies show muscle activity in the jaw jumps 3.1 times during headache episodes.
- Dehydration: When your blood becomes too concentrated (serum osmolality above 295 mOsm/kg), it can trigger pain signals. That’s why drinking water regularly - not just when you’re thirsty - matters.
Here’s the twist: only 22% of headaches labeled as ‘stress-related’ actually happen during high-stress moments. Most occur during the recovery phase - after a big deadline, a busy weekend, or even a vacation. Your body’s drop in stress hormones after prolonged tension is what flips the switch.
How to Stop the Cycle: Prevention That Works
Prevention isn’t about avoiding triggers completely. It’s about reducing your brain’s sensitivity over time.
Cognitive Behavioral Therapy (CBT)
CBT isn’t just ‘talking about stress.’ It’s a structured, evidence-based program that rewires how your brain responds to pain. In a 2021 JAMA Neurology study, patients who did 12 weeks of CBT cut their headache days by 41%. The techniques? Learning to recognize early warning signs, changing how you react to pain, and using relaxation training to calm the nervous system. It’s not a quick fix - but it’s the most durable treatment you can get.
Physical Therapy
Not all physical therapy is the same. For CTH, you need a specialist trained in craniocervical exercises - not just general neck stretches. These focus on strengthening the deep neck flexors, which support your head and reduce strain on the overworked muscles. One study showed 12 sessions of this specific therapy reduced headache frequency by 53%. The catch? Only about 12% of physical therapists in the U.S. have this certification. Ask if they’ve treated cervicogenic headaches before.
Mindfulness and Stress Management
Just 15 minutes a day of mindfulness meditation - focusing on your breath, without judgment - can lower cortisol by 29% in eight weeks. Apps like Headspace or Calm help, but even free YouTube guided meditations work. The key is consistency. Miss a day? It’s okay. Just start again.
Posture Correction
When your head juts forward more than 4.5 centimeters beyond your spine - common when working at a desk - your suboccipital muscles work 2.8 times harder. That’s like carrying a 10-pound weight on your neck all day. Adjust your monitor so the top is at eye level. Use a supportive chair. Set reminders to roll your shoulders back every hour. Small changes add up.
Medications: What Actually Works (and What Doesn’t)
Acute painkillers like ibuprofen or aspirin can help for occasional headaches. But if you’re taking them more than 14 days a month, you risk medication-overuse headache - a vicious cycle where the medicine itself causes more headaches.
Preventive Medications
For chronic cases, daily preventive meds are often needed. The gold standard is amitriptyline, a tricyclic antidepressant. It’s not for depression - it’s for pain. Starting at 10mg at night, it’s slowly increased to 25-50mg. About half to two-thirds of people see a 50% reduction in headache days within six weeks. Side effects? Dry mouth, drowsiness, and weight gain (on average, 2.3kg). Many drop out because of this.
A better-tolerated alternative is mirtazapine. A 2022 trial found it was just as effective as amitriptyline but with fewer side effects. The trade-off? It can make you ravenous. If you’re okay with increased appetite, it’s a strong option.
What Doesn’t Work
- Botox: FDA-approved for migraines, but not for tension headaches. Don’t waste your money.
- Muscle relaxants (like cyclobenzaprine): No strong evidence they help CTH. They cause drowsiness and dependency. Avoid unless under strict supervision.
- Opioids: Zero benefit. High risk of addiction. Never use for CTH.

When to See a Doctor - And What to Ask For
If you’re having headaches on 10 or more days a month, it’s time to see a specialist - not just your GP. A neurologist or headache specialist will ask for a detailed headache diary. Apps like Migraine Buddy or even a simple notebook work. Track: date, time, duration, intensity (1-10), triggers, meds taken, sleep, caffeine, stress levels.
Ask for a neurological exam. It should take at least 15 minutes. They’ll check your vision, reflexes, neck movement, and pressure points. No scan is needed unless there are red flags: sudden severe headache, vision loss, weakness, or confusion.
Don’t accept being told it’s ‘just stress.’ Say: ‘I’ve been tracking my headaches for three months. I meet the ICHD-3 criteria for chronic tension headache. Can we discuss prevention strategies?’
What’s Next: New Treatments on the Horizon
Research is moving fast. The FDA recently fast-tracked atogepant - a drug originally for migraines - for use in CTH. Early trials showed patients had 5.1 fewer headache days per month. That’s huge.
Other promising areas include occipital nerve stimulation (a tiny device implanted behind the neck that sends gentle pulses) and gut-brain research. People with CTH have been found to have lower levels of a specific gut bacteria linked to inflammation. Probiotics might play a role in future treatment.
By 2027, the International Headache Society is expected to rename CTH as ‘primary headache with central sensitization’ - finally ditching the outdated ‘tension’ label. This shift will help doctors understand it’s a brain disorder, not a muscle problem.
Real Stories, Real Results
One Reddit user, after years of misdiagnosis, started tracking sleep and caffeine. She noticed her headaches spiked every time she slept less than 6.5 hours. By sticking to a bedtime within 20 minutes of her usual time, her headaches dropped from 22 days a month to 9.
Another switched from amitriptyline to mirtazapine. The weight gain stopped, and the headaches halved. He still does 15 minutes of breathing exercises every morning. ‘It’s not magic,’ he wrote. ‘It’s just not ignoring the signals anymore.’
Chronic tension headache isn’t a life sentence. It’s a signal - your brain’s way of saying it’s overwhelmed. Fixing it isn’t about finding one magic pill. It’s about rebuilding your daily habits, calming your nervous system, and treating your brain like the complex organ it is.



12 Comments
Let’s be real - calling this 'tension headache' is like labeling climate change as 'a bit warm.' The term is a relic from when doctors thought pain was just muscles being dramatic. The real issue? Central sensitization. Your brain’s alarm system is stuck on 'fire drill' mode. No amount of foam rollers will fix that. This post? Finally someone with actual neurology creds.
I have this every day. I thought it was because I work too hard. But now I see - it’s my sleep and coffee. I cut my coffee to one cup and started sleeping 7 hours. Headaches dropped. Not magic. Just basics.
To anyone reading this and thinking 'I can’t do CBT or physical therapy' - you don’t have to do it all at once. Start with one thing. Maybe it’s drinking a glass of water when you wake up. Or setting a 20-minute timer to look out the window. Small wins build momentum. You’re not broken. Your nervous system just needs gentle recalibration. I’ve been there. You’ve got this.
So let me get this straight - we’ve been blaming neck muscles for 40 years while the real villain was our brain’s overzealous alarm system? And Botox? Nah, baby. That’s just expensive glitter for people who think pain is a fashion statement. Also, 15 minutes of breathing? Yeah, I’ll do that instead of another ibuprofen. Thanks for the reality check.
Central sensitization. Not tension. End of discussion.
🇺🇸 This is why America needs to stop outsourcing brain science to 'wellness influencers.' This is real medicine. Real data. Real neurology. Not some yoga retreat with a $200 'headache crystal.' If you’re still blaming stress or posture like it’s 1998, you’re part of the problem. Fix your sleep. Cut caffeine. Stop scrolling. This isn’t spiritual - it’s neuroscience. 🧠
Man, I’ve been riding this headache train for years - thought I was just 'tense.' Turns out, I was just a walking nervous system glitch. That bit about cortisol spikes after stress? That’s me. Big presentation on Friday? Headache hits Monday. Not because I'm lazy - because my brain’s still panicking. CBT sounds scary, but honestly? I’d rather rewire my brain than swallow another pill that makes me feel like a zombie. Thanks for writing this like a human, not a textbook.
Dear friends, I want to express my heartfelt appreciation for this deeply thoughtful and scientifically grounded exploration of chronic tension headache. As someone who has walked this path, I wish to encourage you to embrace the gentle, consistent practices outlined herein. With discipline, compassion, and a commitment to holistic well-being, transformation is not only possible - it is inevitable. May you find peace in every breath.
Okay but like - is this just central sensitization or is it also like… neuroinflammation? I read this paper last year about microglial activation in CTH and like… the gut-brain axis thing? I think we’re missing the microbiome angle. Also, have you considered that some of the 'triggers' are just epigenetic noise? Like, maybe your mom’s stress during pregnancy primed your trigeminal nucleus? Just saying. 🤔
Central sensitization is a symptom, not a mechanism. The real pathology is maladaptive neuroplasticity in the periaqueductal gray and rostral ventromedial medulla, driven by glutamatergic NMDA receptor hyperactivity and downregulation of descending inhibitory serotonergic pathways. CBT? Fine. But you need pharmacologic modulation of cortical excitability - like gabapentinoids or SNRIs - to reset the gain. Also, sleep hygiene is irrelevant if your circadian rhythm is phase-delayed due to blue light exposure post-sunset. Fix the zeitgeber first.
Okay, so I’ve been dealing with this for like… 12 years? And honestly? I tried everything. Massages, acupuncture, chiropractors, essential oils, biofeedback, even a $400 'headband that vibrates' - none of it worked. Then I started tracking my sleep and caffeine - like, literally writing it down in a notebook - and I realized I was drinking 3 espressos a day and sleeping 5 hours on weekdays, then binge sleeping 10 hours on weekends. That rollercoaster? That was the trigger. I cut caffeine to one cup before noon, went to bed at 11 p.m. every night, and started doing those deep neck flexor exercises. It’s been 6 months. Headaches? Down 80%. I’m not saying it’s easy. I’m saying it’s worth it. You’re not broken. You’re just out of sync. And syncing up? That’s the work. But it’s doable. I’m proof.
lol i just read this whole thing and realized… i’ve been doing all the right things but still get headaches. maybe my brain just likes to be dramatic? also i think i’m addicted to ibuprofen. whoops. 😅