What’s the real difference between a TIA and a stroke?
It’s not about whether symptoms go away. It’s about whether brain tissue is permanently damaged. A TIA-transient ischemic attack-is often called a ‘mini-stroke,’ but that term is misleading and dangerous. If your face droops, your arm goes numb, or your speech slurs-even if it all clears up in 20 minutes-you just had a neurological emergency. The brain doesn’t recover because the problem went away. It recovered because the blockage cleared before it could kill brain cells. That doesn’t mean you’re safe. It means you’re in extreme danger.
Same symptoms, different outcomes
TIA and stroke look identical. You can’t tell them apart by how they feel. Both cause sudden:
- Face drooping on one side
- Weakness or numbness in one arm or leg
- Slurred or confused speech
- Blurred or lost vision in one or both eyes
- Dizziness, loss of balance, or sudden severe headache
The only difference? In a stroke, these symptoms don’t vanish. In a TIA, they usually fade within minutes-often under an hour. But here’s the catch: 35% of people who think they had a TIA actually had a minor stroke. Their symptoms disappeared, but brain scans show permanent damage. That’s why doctors now rely on MRI, not how long symptoms lasted, to decide what happened.
Why calling it a ‘mini-stroke’ can kill you
People say, ‘It’s not a real stroke because it went away.’ That’s the exact mindset that gets people killed. If you ignore a TIA, you have a 20% chance of having a full stroke within 90 days. Half of those strokes happen in the first two days. That’s not a warning. That’s a countdown. A 2021 study in Stroke Journal put it bluntly: ‘TIA is not a warning-it’s an actual stroke event that resolved spontaneously.’
Think of it like a fire alarm. If the alarm goes off and then turns off because someone turned off the power, you don’t say, ‘Oh, it was just a false alarm.’ You check the building. A TIA is your brain’s fire alarm. It’s screaming that blood flow is failing. If you ignore it, the next fire won’t be stopped by luck.
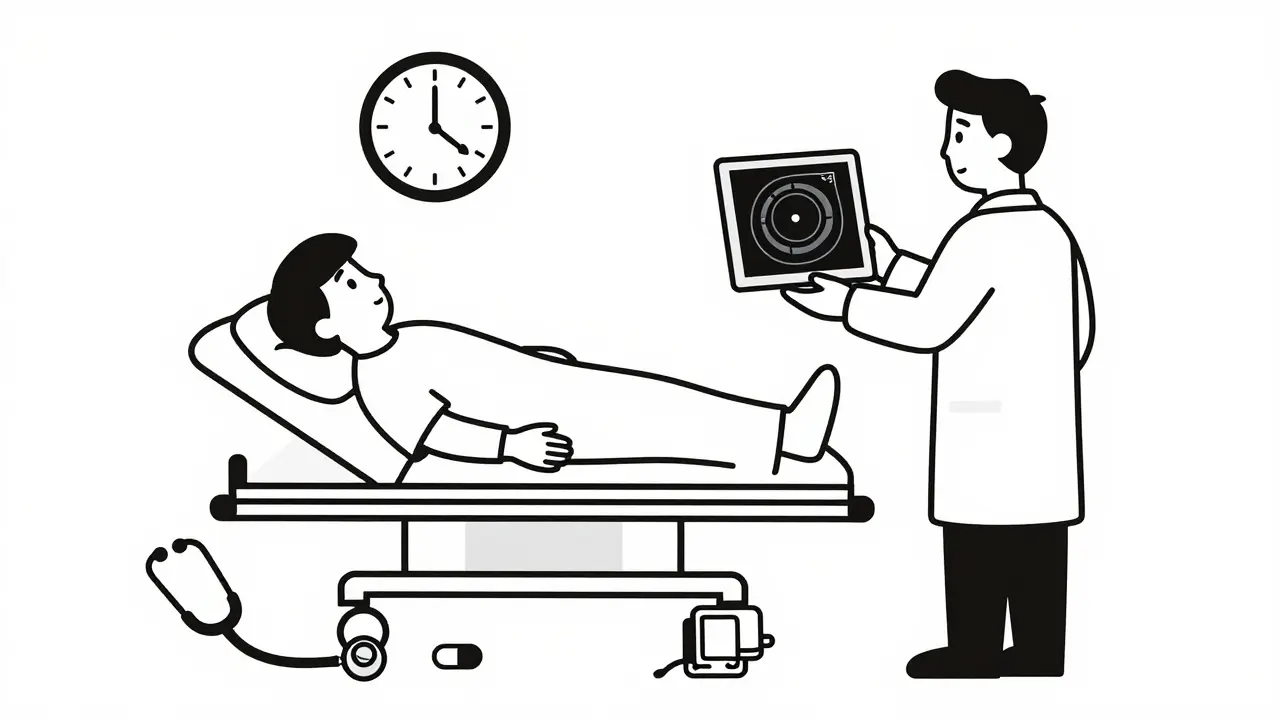
How doctors tell them apart
It’s not guesswork. Emergency rooms use a strict protocol:
- Immediate non-contrast CT scan: Rules out bleeding in the brain.
- Diffusion-weighted MRI within 24 hours: The gold standard. Detects even tiny areas of dead brain tissue.
- ABCD2 score: A simple risk calculator based on Age, Blood pressure, Clinical symptoms, Duration of symptoms, and Diabetes.
For example: A 68-year-old with high blood pressure, arm weakness lasting 45 minutes, and type 2 diabetes scores a 6 out of 7. That’s high risk. Their chance of stroke in two days? Over 8%. That’s not a ‘maybe.’ That’s a ‘do something now.’
And here’s the kicker: 40% of patients initially diagnosed with TIA are later found to have had a minor stroke after MRI. That means doctors were wrong-based on symptoms alone. Imaging doesn’t lie.
What to do the moment symptoms appear
Forget ‘wait and see.’ If you or someone else has any stroke-like symptom, call 911-even if it’s gone. The BE FAST acronym works for both TIA and stroke:
- Balance: Sudden dizziness or loss of coordination
- Eyes: Vision changes in one or both eyes
- Face: One side drooping when smiling
- Arm: One arm drifting down when raised
- Speech: Slurred, strange, or hard to understand
- Time: Call 911 immediately
Don’t drive yourself. Don’t wait to see if it comes back. Ambulances can start treatment en route. Hospitals can activate stroke teams before you arrive. Time saved is brain saved.
Treatment after a TIA: It’s not optional
After a TIA, you’re not done. You’re just getting started. The goal isn’t to treat the past event-it’s to prevent the next one. Here’s what happens next:
- Aspirin within 24 hours: Reduces stroke risk by 60%.
- Dual antiplatelet therapy: Aspirin + clopidogrel for 21-30 days cuts risk by 80% compared to aspirin alone.
- High-intensity statin: Atorvastatin 80 mg daily lowers cholesterol aggressively to stabilize artery plaques.
- Blood pressure control: Target under 140/90 mmHg. Often requires multiple medications.
Studies show that if you get all of this started within 48 hours, your risk of stroke drops from over 10% to under 2% in 90 days. Delay treatment by a week? Your risk stays high. That’s why top hospitals now have TIA clinics that see patients the same day-even if they’re feeling fine.
Why most people miss the warning
One in three people who have a TIA don’t seek help right away. Why? Because they think, ‘It’s gone. I’m fine.’ The CDC found that 31% of TIA patients wait more than 24 hours to get checked. That’s like ignoring a cracked windshield and hoping the glass won’t shatter on the highway.
Older adults are especially at risk. The median age for a TIA is 69. Many assume dizziness or slurred speech is just ‘getting older.’ It’s not. It’s a sign your arteries are failing. And if you’re diabetic, have high blood pressure, or smoke? Your risk doubles.
What’s new in TIA care (2025)
Things are changing fast:
- AI risk tools: New algorithms analyze MRI scans and patient data to predict stroke risk within 7 days with 92% accuracy.
- Telemedicine TIA clinics: 68% of major stroke centers now offer same-day virtual evaluations.
- Point-of-care blood tests: A biomarker called GFAP is being tested to detect brain injury within 15 minutes-could replace waiting for MRI in some cases by 2026.
- Hospital penalties: Medicare now fines hospitals if more than 20% of TIA patients have a stroke within 30 days. That’s forcing real change.
These aren’t future ideas. They’re happening now. The goal? Reduce 90-day stroke rates from 10% to under 2%-and we’re getting close.
What you need to remember
There’s no such thing as a ‘minor’ TIA. It’s not a warning. It’s a signal that your brain is one clot away from permanent damage. If you ignore it, you’re gambling with your life-and your future. The science is clear: act fast, get scanned, start treatment, and never assume symptoms going away means you’re safe.
Every minute counts. Every decision matters. Your brain doesn’t get second chances.
Can a TIA happen without symptoms?
No. By definition, a TIA causes noticeable neurological symptoms-like weakness, speech trouble, or vision loss-that come on suddenly. But some people have what’s called a ‘silent’ stroke, which shows up on an MRI with no obvious symptoms. That’s different from a TIA. A TIA always has symptoms, even if they disappear quickly.
If my TIA symptoms are gone, do I still need to go to the hospital?
Yes. Absolutely. Even if you feel 100% fine, you need emergency evaluation. The damage isn’t in how you feel-it’s in what’s happening inside your arteries. Up to 20% of people who have a TIA will have a stroke within 90 days, and half of those happen within 48 hours. Waiting means risking permanent disability or death.
Is a TIA the same as a mini-stroke?
No. ‘Mini-stroke’ is a misleading term used by the public, not doctors. It suggests the event isn’t serious. But a TIA is a full-blown interruption of blood flow to the brain. The only reason there’s no permanent damage is because the blockage cleared quickly. It’s not minor-it’s a major red flag.
Can you have a TIA and not know it?
No. A TIA always causes sudden, noticeable symptoms. If you didn’t notice anything-no weakness, no slurred speech, no vision changes-you didn’t have a TIA. But you might have had a silent stroke, which shows up on MRI and has no obvious signs. Silent strokes still increase your risk of future stroke and dementia.
How long after a TIA is the stroke risk highest?
The highest risk is in the first 48 hours. About 5% of people have a stroke within two days. That’s why guidelines say you need to be evaluated within 24 hours, and high-risk patients should be seen within 12 hours. Delaying care increases your risk dramatically.
Does aspirin help after a TIA?
Yes-quickly. Taking 325 mg of aspirin within 24 hours of a TIA reduces your risk of a future stroke by 60%. But aspirin alone isn’t enough. For high-risk patients, doctors add clopidogrel for 21-30 days, along with a strong statin and blood pressure control. Aspirin is a start, not the full treatment.
Can a TIA be seen on a CT scan?
Usually not. A standard CT scan can rule out bleeding, but it can’t detect the tiny changes from a TIA. That’s why MRI with diffusion-weighted imaging is required. It’s 99% accurate at spotting even small areas of brain injury. If your CT was normal but you had symptoms, you still need an MRI.
Are TIAs more common in older people?
Yes. The average age for a TIA is 69, compared to 74 for a full stroke. But they’re increasing in younger adults too-especially those with obesity, diabetes, high blood pressure, or smoking habits. Anyone with these risk factors should know the warning signs, no matter their age.

11 Comments
Just had my dad go through this last year. He ignored the numbness in his arm for 3 hours because he thought it was ‘just a pinched nerve.’ Turned out it was a TIA. He’s fine now because he finally went in-but I’ll never forget how close we came. If you feel even a little off, don’t wait. Call 911. No excuses.
u r all weak. in nigeria we dont have MRI or ambulances. we just pray and keep walking. if u get stroke u die. if u dont u live. no time for fancy scans. ur westen medical drama is pathetic.
The 35% misdiagnosis rate is the real story. Most ERs still rely on symptom duration. That’s outdated. MRI is the only truth. No ifs ands or buts. If you’re not imaging within 24 hours you’re gambling. And yes the 20% 90 day stroke risk is real. No sugarcoating.
I used to think TIA was just a scare tactic. Then my sister had one and the docs said ‘you’re lucky’-and I believed them. Turns out she had permanent micro-injuries on the MRI. I wish someone had told us that sooner. This post? It’s a wake-up call. Please share it with your family. Especially older folks who think ‘it’s just aging’.
The real tragedy isn't the TIA it's the collective denial of mortality. We treat the body like a machine that can be reset. But the brain doesn't forgive. It remembers every micro-infarct. And we? We keep ignoring the alarm because we're too busy scrolling. This isn't medicine. It's metaphysics.
Thank you for this clear, evidence-based breakdown. I’ve worked in neurology for 18 years, and I still see patients who say, ‘It went away, so I didn’t come in.’ The ‘mini-stroke’ myth is dangerously pervasive. Please, if you’re reading this: if your face droops-even for 10 seconds-call 911. Don’t text your cousin. Don’t Google it. Call 911.
Wait so if the symptoms go away but MRI shows damage, is that still called a TIA? Or is it a stroke? I’m confused because the article says TIA means no permanent damage but then says 35% of people who think they had a TIA actually had a stroke? So what’s the definition now?
The brain is like a phone. One glitch doesn’t mean it’s broken. But if it keeps glitching? You replace it. TIA is the phone saying ‘battery critical.’ You don’t ignore it because it turned off. You charge it before it dies forever.
I’m 34 and had a TIA last year. I thought it was anxiety. Turns out I had a patent foramen ovale and high LDL. Now I take aspirin, statin, and run 5Ks. No one warned me. I’m so glad I found this. To anyone young reading this: don’t assume you’re too young. It can happen to anyone. Get checked.
I HATE that people say 'it went away so it's fine'!! That's like saying 'the fire alarm stopped so the house isn't burning'!! I had my mom's best friend die from stroke after she 'just had a little dizzy spell'!! THEY LIE TO YOU AND THEN THEY DIE AND NO ONE CARES!!
Aspirin within 24 hours? I didn’t know that. I thought you had to wait for the doctor. So if I feel something even for a minute I should just take one right away?