Osteonecrosis of the Jaw Risk Calculator
This calculator estimates your risk of developing osteonecrosis of the jaw (ONJ) based on your medication type and duration of use. ONJ is rare but serious for some patients taking certain bone medications.
Your Risk Assessment
| Estimated Risk: | 0% |
| Recommended Actions: |
When you're taking medication for osteoporosis or cancer that's spread to your bones, you're probably focused on how it's helping you-stopping fractures, slowing tumor growth, improving your quality of life. But there’s a silent, serious risk hiding in your mouth: osteonecrosis of the jaw (ONJ), also called medication-related osteonecrosis of the jaw (MRONJ). It’s rare, but when it happens, it’s bad. And the worst part? It often starts with something that feels like a simple toothache or gum infection.
What Exactly Is Osteonecrosis of the Jaw?
Imagine your jawbone slowly dying because it can’t heal itself. That’s what ONJ is. The bone becomes exposed through the gums and doesn’t heal for eight weeks or longer. It doesn’t just happen out of nowhere-it’s triggered by medications that stop bone from breaking down and rebuilding. These drugs, like bisphosphonates and denosumab, are lifesavers for people with osteoporosis or cancer. But they also shut down the natural repair system in your jaw. Without that repair, even small injuries-a tooth extraction, a denture rubbing too hard, or just brushing too aggressively-can lead to dead bone sticking out in your mouth.
This isn’t just a theory. The National Institute of Dental and Craniofacial Research (NIDCR) says the diagnosis requires one clear sign: exposed bone in the jaw that lasts more than eight weeks. And it’s not rare in high-risk groups. For someone on oral bisphosphonates for osteoporosis, the chance is about 1 in 10,000 to 1 in 100,000 per year. But for someone getting monthly IV zoledronate for bone cancer? That risk jumps to 1 in 10 to 1 in 100. That’s a 1,000-fold difference.
The Warning Signs: Don’t Wait for the Worst
Most people don’t realize they’re at risk until it’s too late. The early signs are easy to miss because they look like common dental problems. But if you’re on one of these medications, pay attention:
- Pain or swelling in your jaw or mouth - This is the most common symptom, reported in 87% of cases. It doesn’t always mean an infection, but it shouldn’t be ignored.
- Delayed healing after a tooth extraction - If your gums haven’t closed up or are still bleeding after two weeks, that’s not normal. About 76% of ONJ cases follow a dental procedure.
- Loose teeth with no obvious cause - If you’re not a gum disease patient and suddenly teeth feel wobbly, your jawbone might be weakening.
- Visible bone in your mouth - This is the defining sign. You might see a grayish, hard piece of bone sticking out near a tooth socket or under a denture.
- Pus or foul-smelling discharge - A sign of infection, but not the kind that antibiotics fix easily. This happens in 58% of cases.
- Numbness or heaviness in your jaw - If your lower lip or chin feels numb, or your jaw feels unusually heavy, it could mean nerve damage from dead bone pressing on it. Seen in 42% of patients.
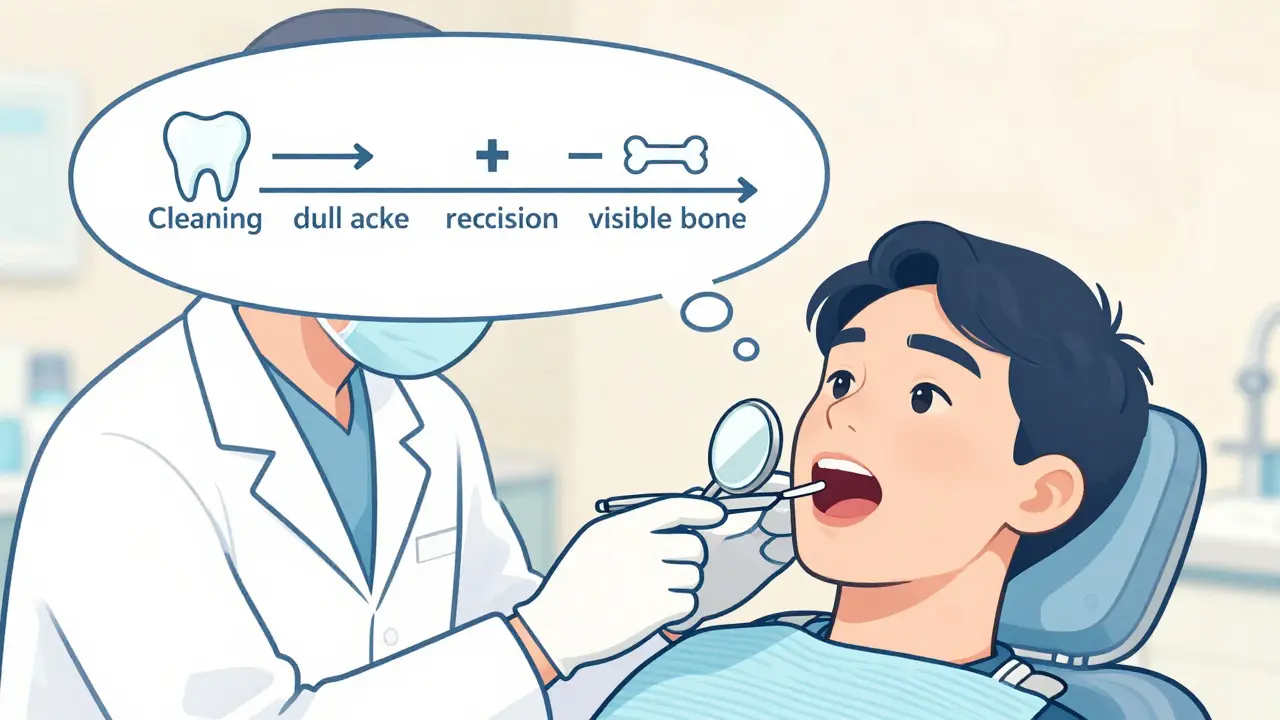
These symptoms don’t show up overnight. They creep in. A patient on alendronate (Fosamax) might notice a dull ache after a cleaning. They think it’s just sensitivity. A month later, the gum around a tooth pulls back. Two months later, they see bone. By then, it’s stage 2 or 3. Early detection is everything.
Which Medications Are Riskiest?
Not all drugs are created equal. The biggest culprits are:
- IV bisphosphonates - Zoledronate (Reclast, Zometa) and pamidronate. Used for cancer that’s spread to bone. Highest risk.
- Oral bisphosphonates - Alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva). Used for osteoporosis. Risk is very low, but it’s not zero.
- Denosumab (Prolia, Xgeva) - A newer drug that works differently than bisphosphonates, but still suppresses bone turnover. Risk is similar to oral bisphosphonates for osteoporosis, but higher in cancer doses.
- Romosozumab - A newer osteoporosis drug. Early data suggests lower risk than bisphosphonates, but long-term studies are still ongoing.
Here’s the key: IV drugs are 100 to 1,000 times riskier than oral ones. A patient on monthly IV zoledronate for breast cancer has a 5-10% chance of developing ONJ over 3 years. Someone on Fosamax for 5 years? Less than 0.015%. That’s why prevention strategies are totally different depending on how you take the drug.
Dental Procedures: The Real Trigger
Here’s what most people don’t know: Routine cleanings, fillings, and crowns are generally safe. The real danger comes from invasive procedures-especially tooth extractions. Studies show that in patients on bisphosphonates, the risk of ONJ after an extraction is 3.2%. In people not on these drugs? Just 0.05%. That’s a 64-fold increase.
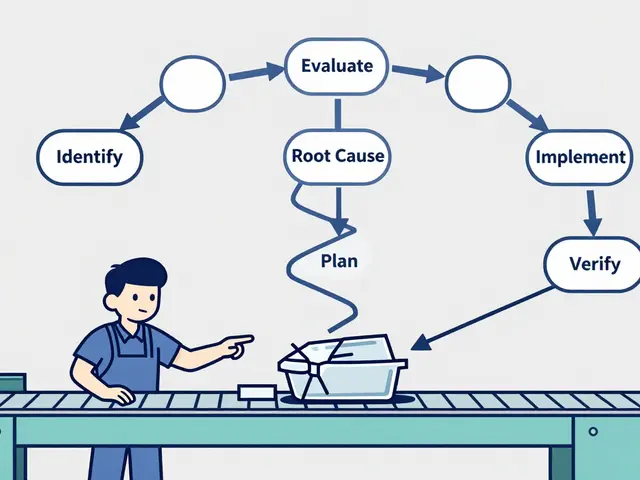
And it’s not just extractions. Dentures that rub too hard, root canals, or even deep scaling can trigger it. That’s why timing matters. If you’re starting IV bisphosphonates or denosumab for cancer, you need a full dental exam 4 to 6 weeks before your first dose. Get everything fixed-pull teeth, treat infections, adjust dentures-before the drug shuts down your healing. If you’re already on the medication, don’t panic. But if you need a tooth pulled, talk to your doctor about a temporary pause. For IV drugs, a 2- to 3-month break can reduce risk significantly.
What You Can Do to Prevent It
You can’t stop the medication if you need it. But you can drastically lower your risk:
- Get a dental checkup before starting - If you’re about to begin IV bisphosphonates or denosumab, schedule a full exam. X-rays, gum check, denture fit-all of it. Do this 4-6 weeks before treatment starts.
- Tell every dentist you see - Even if you’re on oral osteoporosis meds. Most dentists still don’t ask. A 2022 study found 73% of ONJ patients said their dentist never asked about their medications.
- Use chlorhexidine mouthwash - A 2021 trial showed rinsing twice daily with 0.12% chlorhexidine reduces ONJ risk by 37% in high-risk patients. It’s cheap, easy, and available over the counter.
- Keep your mouth clean - Brush twice a day, floss daily. Poor oral hygiene increases risk. Diabetes, smoking, and gum disease make it worse.
- Don’t delay dental care - Avoiding cleanings because you’re scared of ONJ? That’s dangerous. Routine care is safe. It’s invasive procedures you need to plan for.
What Happens If It’s Not Caught Early?
Left untreated, ONJ doesn’t just hurt-it can destroy your jaw. Bone fragments can break off. Infections spread. You might lose teeth. In severe cases, you need surgery to remove dead bone, which can leave you with holes in your jaw, difficulty eating, or even facial disfigurement. Some patients need long-term antibiotics. Others never fully recover.
But here’s the good news: If caught early, it can be managed. Stage 1 ONJ (just exposed bone, no infection) can often be treated with mouth rinses, antibiotics, and avoiding trauma. New research from UCSF shows that teriparatide (Forteo), a bone-building drug, helped 78% of early-stage ONJ patients heal within 6 months-compared to only 32% with standard care. That’s a game-changer.
Why So Many People Miss the Signs
Most patients don’t know they’re at risk. A survey from the National Osteoporosis Foundation found 65% of cancer patients weren’t told about ONJ before starting IV meds. Dentists, too-especially in private practices-aren’t always trained to recognize the early signs. Only 68% of private clinics follow pre-treatment screening guidelines, compared to 94% at university dental centers.
And when patients do notice symptoms, they often blame it on a cavity or gum disease. One Reddit user shared: "I had pain for 8 months. Went to three dentists. They all said it was an abscess. Only the fourth one asked about my osteoporosis meds." That’s not unusual.
The Bottom Line
ONJ is rare. For most people on oral osteoporosis meds, the benefits of preventing a broken hip far outweigh the tiny risk of jaw death. But if you’re on IV drugs for cancer, or you’ve been on oral meds for more than 3 years, you need to be smart about your dental care.
Don’t wait for pain. Don’t assume your dentist knows. Don’t skip checkups because you’re scared. Do this: Tell every dental provider you’re on a bisphosphonate or denosumab. Get a full exam before starting high-risk meds. Use mouthwash. Keep your gums healthy. And if you notice bone showing up or healing that won’t happen? See a specialist-now.
The goal isn’t to scare you. It’s to make sure you stay healthy-inside and out. Your jawbone doesn’t scream for help. It whispers. Listen before it’s too late.
Can you get osteonecrosis of the jaw from taking oral bisphosphonates like Fosamax?
Yes, but it’s extremely rare. For people taking oral bisphosphonates for osteoporosis, the risk is between 0.001% and 0.01% over several years. That’s roughly 1 in 10,000 to 1 in 100,000 patients per year. Most cases occur after dental surgery, especially extractions, and are more likely after 3-4 years of continuous use. The benefits of preventing fractures still far outweigh this tiny risk for most people.
Is osteonecrosis of the jaw the same as a regular tooth infection?
No. A tooth infection is caused by bacteria and usually responds to antibiotics and drainage. ONJ is caused by dead bone tissue that can’t heal because medications block bone turnover. It doesn’t go away with standard treatment. Signs include exposed bone lasting more than 8 weeks, lack of healing after extraction, and pain that doesn’t improve with antibiotics. If you’re on high-risk meds and have these symptoms, you need a specialist evaluation.
Should I stop my osteoporosis medication to avoid jaw problems?
No-not unless your doctor tells you to. Stopping bisphosphonates or denosumab can increase your risk of fractures, which can be life-threatening, especially in older adults. The risk of ONJ is very low compared to the risk of breaking a hip or spine. Instead of stopping, focus on prevention: get dental checkups before starting treatment, tell your dentist about your meds, and avoid invasive procedures unless absolutely necessary.
Can I still get my teeth cleaned if I’m on these medications?
Yes, routine dental cleanings and fillings are safe. In fact, keeping your mouth healthy lowers your risk of ONJ. The danger comes from procedures that cut into bone, like extractions or implants. Regular cleanings help prevent gum disease, which can be a trigger. Always tell your hygienist you’re on a bisphosphonate or denosumab so they can take extra care.
How long after starting the medication does ONJ usually develop?
It varies. For cancer patients on IV bisphosphonates, most cases occur within 12 months of starting treatment, especially after a dental procedure. For osteoporosis patients on oral meds, ONJ typically develops after 3-4 years of continuous use. The risk increases the longer you take the drug. That’s why pre-treatment dental exams are so important-they catch problems before the medication starts.
Are there any new treatments for ONJ?
Yes. Traditional treatment focuses on managing infection and removing dead bone. But newer research shows promise with teriparatide (Forteo), a bone-building drug. A 2023 study found it helped 78% of early-stage ONJ patients heal, compared to 32% with standard care. Also, the NIH is testing a personalized risk tool called the Osteonecrosis Prediction Algorithm (OPA), which uses genetic and dental data to predict who’s most at risk. These tools could change how we prevent ONJ by 2025.
For more information, refer to guidelines from the American Dental Association (ADA) and the American College of Rheumatology. Always consult your doctor and dentist before making changes to your treatment plan.