COPD Medication Schedule Calculator
How to Use This Calculator
This tool calculates your dosing schedule based on clinical guidelines. Ipratropium bromide is typically prescribed as 2 puffs every 4-6 hours. Maximum daily limit is 8 puffs (4 doses).
Important: Always follow your doctor's specific instructions. This calculator is for informational purposes only.
Key Takeaways
- Ipratropium bromide is a short‑acting anticholinergic bronchodilator that improves airflow in COPD patients.
- It is most effective when used regularly or as rescue therapy for sudden breathlessness.
- Guidelines (GOLD) place ipratropium as a first‑line reliever, often in combination with a β2‑agonist.
- Typical dosing is 2 puffs (0.5 mg) every 4‑6 hours via metered‑dose inhaler (MDI) or nebulizer.
- Side‑effects are usually mild (dry mouth, cough) but clinicians should monitor for paradoxical bronchospasm.
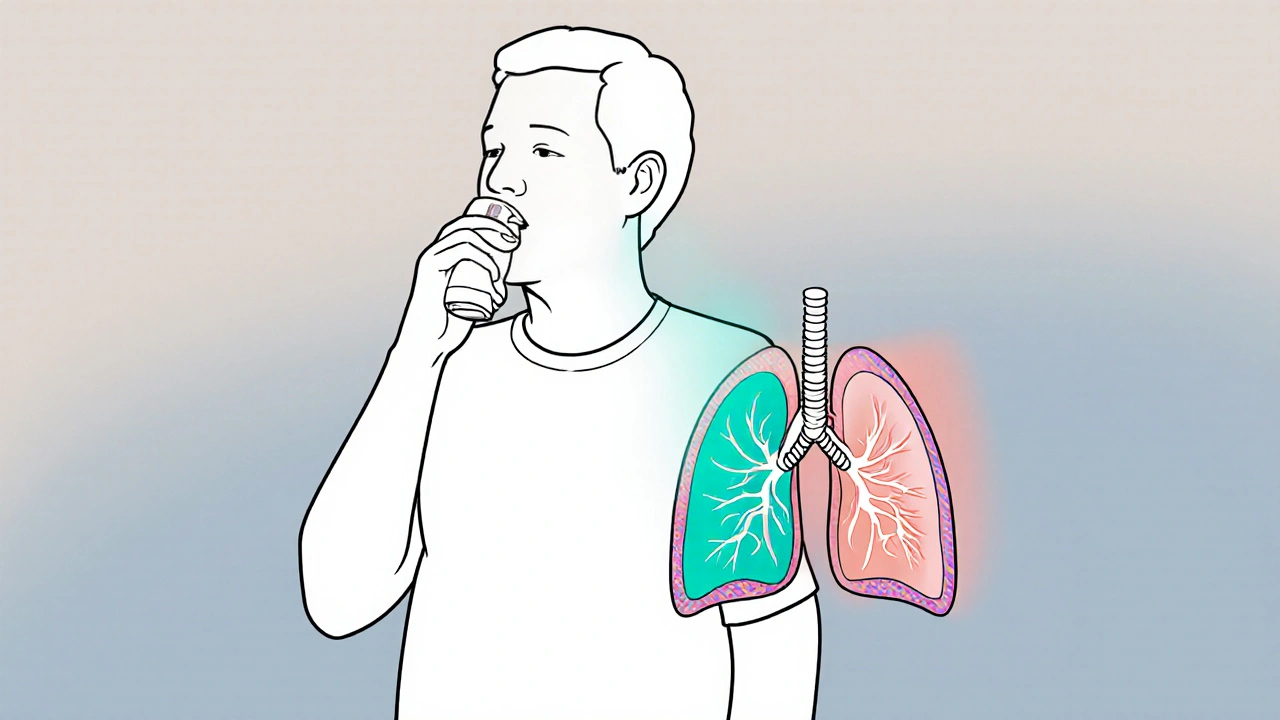
What is Ipratropium Bromide?
Ipratropium Bromide is a short‑acting muscarinic antagonist (SAMA) that relaxes airway smooth muscle by blocking acetylcholine receptors. By preventing bronchoconstriction, it widens the airways and eases breathing.
First approved in the 1980s, ipratropium is delivered via metered‑dose inhaler (MDI), dry‑powder inhaler (DPI) or nebulizer solution. Its rapid onset (within minutes) and modest duration (about 4‑6 hours) make it suitable for rescue use and for twice‑daily maintenance in milder COPD.
Understanding COPD
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by airflow limitation that is not fully reversible. The two main pathological components are chronic bronchitis (airway inflammation) and emphysema (alveolar destruction).
Patients experience persistent cough, sputum production, and episodes of worsening breathlessness called exacerbations. Lung‑function is commonly measured by forced expiratory volume in one second (FEV1), which declines over time.
How Ipratropium Works in COPD
Ipratropium’s anticholinergic action blocks the M3 muscarinic receptors on airway smooth muscle. In COPD, parasympathetic tone is heightened, leading to excessive acetylcholine release and bronchoconstriction. By inhibiting this pathway, ipratropium provides several clinical benefits:
- Improved FEV1: studies show a 5‑10 % rise in FEV1 within 15 minutes of inhalation.
- Reduced airway resistance, especially during night‑time and early‑morning periods.
- Decreased mucus hypersecretion, thanks to its effect on glandular secretions.
- Lower risk of acute exacerbations when used consistently.
The drug’s rapid onset complements fast‑acting β2‑agonists (e.g., albuterol) that work via a different mechanism, providing additive bronchodilation.
Dosage, Formulations & Administration Tips
Typical dosing for COPD is 2 puffs (0.5 mg per puff) every 4‑6 hours, not exceeding 8 puffs per day. The medication is available as:
- MDI (metered‑dose inhaler) - the most common format for ambulatory patients.
- Solution for nebulization - useful for severe dyspnea or in patients who cannot coordinate inhaler actuation.
- DPI (dry‑powder inhaler) - less common, but an option for those preferring breath‑actuated devices.
Key administration pointers:
- Shake the MDI vigorously for at least 5 seconds before each use.
- Exhale fully, place the mouthpiece between lips, and inhale slowly while actuating.
- Hold breath for 5‑10 seconds to allow maximal drug deposition.
- Rinse mouth after each dose to reduce dry‑mouth sensation.
Comparison with Long‑Acting Anticholinergics (LAMA)
| Attribute | Ipratropium Bromide (SAMA) | Tiotropium (LAMA) |
|---|---|---|
| Onset of action | Within 5‑15 minutes | Within 30‑60 minutes |
| Duration | 4‑6 hours | 24 hours (once‑daily) |
| Typical dosing | 2 puffs q4‑6h (max 8 puffs/day) | 1‑2 puffs once daily |
| Primary indication | Relief & mild maintenance | Maintenance therapy for moderate‑to‑severe COPD |
| Side‑effect profile | Dry mouth, cough, throat irritation | Dry mouth, constipation, urinary retention (rare) |
Both agents belong to the anticholinergic class, but their pharmacokinetics guide different roles. Ipratropium is ideal for quick relief and for patients who cannot tolerate a daily LAMA, while tiotropium is the backbone of maintenance therapy in GOLD stage 2‑4.
Safety Profile & Common Side Effects
Adverse events are generally mild and reversible. The most frequently reported effects are:
- Dry mouth (xerostomia) - mitigated by sipping water after each dose.
- Throat irritation or cough - often lessened by using a spacer with the MDI.
- Rare paradoxical bronchospasm - requires immediate discontinuation and alternative therapy.
Systemic absorption is minimal, so systemic anticholinergic effects (e.g., urinary retention, tachycardia) are uncommon. However, clinicians should exercise caution in patients with narrow‑angle glaucoma or severe urinary outflow obstruction.

Position in GOLD Guidelines & Combination Strategies
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 report categorizes treatments by symptom burden and exacerbation risk. Ipratropium appears in two key contexts:
- As a rescue bronchodilator-combined with a short‑acting β2‑agonist (SABA) like albuterol. This dual‑reliever strategy provides additive bronchodilation and is recommended for all GOLD groups.
- As part of maintenance-especially when patients cannot tolerate a LAMA or have predominately bronchoconstrictive symptoms. It may be paired with a long‑acting β2‑agonist (LABA) or a low‑dose inhaled corticosteroid (ICS) for added control.
Evidence from large randomized trials (e.g., UPLIFT, TORCH) indicates that adding ipratropium to LABA/ICS regimens reduces exacerbation rates by roughly 10‑12 % compared with LABA/ICS alone.
Practical Tips for Clinicians & Patients
- Assess inhaler technique at every visit; even small errors greatly reduce drug deposition.
- For patients with dexterity problems, recommend a nebulizer solution or a spacer device.
- Encourage a rescue action plan: use 2 puffs of ipratropium plus 2 puffs of albuterol at the first sign of worsening breathlessness.
- Review medication list for anticholinergic load; avoid stacking with oral antihistamines that may exacerbate dry mouth.
- Monitor lung function (spirometry) every 6‑12 months to gauge treatment response.
Conclusion
When used correctly, Ipratropium bromide offers a reliable, fast‑acting option for COPD patients who need symptom relief without the systemic effects of oral medications. It fits seamlessly into GOLD‑guided step‑wise therapy, either as a standalone reliever or in combination with β2‑agonists and inhaled steroids. Understanding its dosing, safety profile, and place among long‑acting anticholinergics ensures clinicians can tailor treatment to each patient’s severity and lifestyle.
Frequently Asked Questions
Can I use ipratropium with my inhaled corticosteroid?
Yes. Ipratropium can be added to an inhaled corticosteroid (ICS) regimen to improve bronchodilation, especially in patients with frequent symptoms but low exacerbation risk.
How quickly does ipratropium start working?
Onset is typically within 5‑15 minutes, making it suitable for rescue use during sudden breathlessness.
Is ipratropium safe for elderly patients?
Generally yes. Systemic absorption is low, but clinicians should watch for dry mouth and avoid use in patients with narrow‑angle glaucoma.
What’s the difference between ipratropium and tiotropium?
Ipratropium is short‑acting (4‑6 h) and used for relief; tiotropium is long‑acting (24 h) and serves as daily maintenance therapy.
Can I use ipratropium if I’m also on a β2‑agonist?
Absolutely. The two drugs act on different receptors and provide additive bronchodilation when combined.


15 Comments
Hey! I think ipratropium is super handy especially when you need quick relief
just remember the spacer tip.
Great summary! I especially like the reminder about checking inhaler technique at each visit. It’s crucial for getting the most out of any bronchodilator and can really make a difference in symptom control.
Ipratropium works fast and it's cheap.
While the article outlines the pharmacologic benefits of ipratropium bromide, it neglects to address comparative cost‑effectiveness and real‑world adherence challenges. Moreover, the brief mention of paradoxical bronchospasm lacks depth, especially given the potential severity of such events. A more rigorous discussion of patient selection criteria would strengthen the piece.
We can't just shrug off these so‑called "minor" side‑effects. Patients deserve better than a quick fix that leaves them with a dry mouth and throat irritation!
Ipratropium bromide occupies a unique niche in COPD management that is often underappreciated. Its rapid onset of action, typically within five to fifteen minutes, makes it an ideal candidate for rescue therapy. The short‑acting nature also allows clinicians to fine‑tune dosing schedules based on individual symptom patterns. When combined with a short‑acting β2‑agonist, you achieve additive bronchodilation through complementary receptor pathways. This dual‑reliever strategy is endorsed by recent GOLD updates for its efficacy in reducing exacerbation frequency. From a pharmacodynamic standpoint, ipratropium blocks M3 muscarinic receptors, thereby attenuating acetylcholine‑mediated bronchoconstriction. The resulting decrease in airway resistance improves FEV1 values by roughly five to ten percent within minutes. Clinical trials have consistently demonstrated reduced nocturnal symptoms, which is critical for patient quality of life. The medication’s modest side‑effect profile-primarily dry mouth and mild cough-makes it well tolerated even in frail elderly populations. Proper inhaler technique, including a slow inspiratory flow and breath‑hold, maximizes drug deposition and minimizes oropharyngeal deposition. Using a spacer or opting for nebulized delivery can further enhance efficacy in patients with coordination difficulties. Importantly, ipratropium does not exert systemic anticholinergic effects, limiting concerns about urinary retention or glaucoma exacerbation. Nevertheless, clinicians should remain vigilant for paradoxical bronchospasm, albeit rare, and discontinue promptly if it occurs. The drug’s low cost relative to long‑acting anticholinergics also offers a budget‑friendly option for health systems. In summary, ipratropium serves as a versatile tool for both acute symptom relief and adjunct maintenance, bridging the gap between short‑acting bronchodilators and long‑acting agents.
Honestly, it feels like Big Pharma pushed ipratropium to keep us hooked on inhalers. They market it as a miracle rescue, yet the real agenda is to maintain a steady revenue stream.
When we breathe easier, we get a fleeting glimpse of our own fragility; the medication becomes a reminder that health is a delicate balance we must nurture.
The present article provides a concise overview; however, the omission of pharmacoeconomic considerations may limit its applicability in resource‑constrained settings.
Absolutely, Selina. Using a spacer can dramatically improve drug deposition, especially for patients with limited inspiratory flow.
Yeah, that’s the bottom line-quick, cheap, works.
Sure, Andrew, but dry mouth can be mitigated with water, no need to hypee it 😅
I really liked Kristin’s deep dive, though I think a few headings could be clearer. Sorry for any typos!
Good point, Shermaine. Concise summaries help busy clinicians.
Honestly, Theo, the claim that pharma engineers dependence is a stretch; the data supports efficacy without hidden agendas.