
Every year, tens of thousands of seniors end up in emergency rooms-not because of a fall, heart attack, or infection, but because of a medication they were told was safe. For people over 65, the body doesn’t process drugs the way it used to. Liver function slows. Kidneys filter less. Brain receptors become more sensitive. What was a harmless pill at 45 can become dangerous at 75. The question isn’t whether your loved one is taking too many pills-it’s whether any of them are high-risk medications for seniors that should be reviewed or replaced.
What Makes a Medication High-Risk for Older Adults?
It’s not about being ‘strong’ or ‘powerful.’ It’s about how the aging body reacts. A drug that’s fine for a 30-year-old might cause confusion, falls, or even organ damage in someone over 65. The American Geriatrics Society (AGS) keeps a living list called the Beers Criteria, updated every two years, that identifies medications with risks that outweigh benefits for older adults. The latest version, from May 2023, lists 30 classes of drugs and 14 individual medications that should generally be avoided.
These aren’t random picks. Each one has been studied in real-world populations. For example, zolpidem (Ambien®), a common sleep aid, increases the risk of hip fractures by 2.5 times in seniors. Why? Because it lingers in the system. Older adults metabolize it slower, so they wake up groggy, disoriented, and unsteady-even 11 hours after taking it. That’s not just drowsiness; that’s a walking hazard.
Then there’s glyburide, a diabetes drug. It’s cheap and widely prescribed, but it causes severe low blood sugar in nearly 30% of seniors. That’s more than double the rate of safer alternatives like glipizide. A single episode of hypoglycemia can lead to a fall, a hospital visit, or worse. In fact, CMS data shows glyburide leads to 4.2 emergency visits per 100 patients each year.
Top 5 High-Risk Medications to Review Right Now
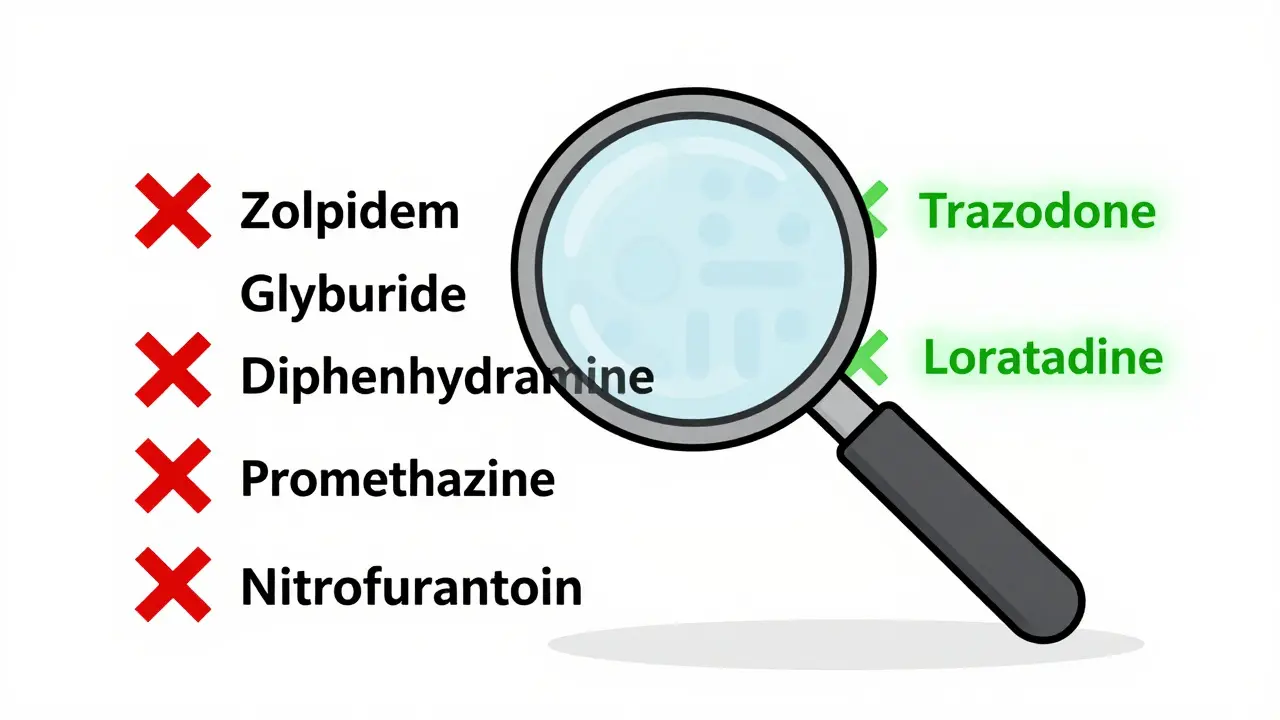
- Zolpidem (Ambien®, Edluar®) - Used for insomnia. Increases fall risk by 82%. Residual sedation lasts up to 11 hours. Alternatives: Trazodone, cognitive behavioral therapy for insomnia (CBT-I).
- Glyburide (Diabeta®, Glynase®) - A sulfonylurea for type 2 diabetes. High risk of dangerous low blood sugar. Glipizide or metformin are safer choices.
- Diphenhydramine (Benadryl®) - Found in sleep aids, allergy meds, and cold remedies. Strong anticholinergic effects. Long-term use raises dementia risk by 54%. Avoid all products with this ingredient.
- Promethazine (Phenergan®) - Used for nausea and allergies. Can cause severe drowsiness, confusion, and even seizures in seniors. Especially dangerous for those with Parkinson’s. Ondansetron is a better option.
- Nitrofurantoin (Macrobid®) - Prescribed for urinary tract infections. Can cause fatal lung damage in people with reduced kidney function (eGFR under 60). Nitrofurantoin should be avoided if kidney function is impaired.
These aren’t outliers. They’re common. You’ll find them in medicine cabinets across the country. Many seniors take them because they were prescribed years ago and no one ever revisited the list.
Anticholinergic Burden: The Silent Killer
One of the most dangerous but overlooked risks is anticholinergic burden. This isn’t about one drug-it’s about the total effect of multiple drugs that block acetylcholine, a brain chemical critical for memory and muscle control.
Drugs like amitriptyline (for nerve pain), oxybutynin (for overactive bladder), and even some cold medicines contain anticholinergic properties. When stacked together, they create a cumulative effect. A score of 3 or higher on the Anticholinergic Risk Scale means high risk. A score of 3+ over 3 years increases dementia risk by 50%.
One 78-year-old woman in a CDC case study took amitriptyline for neuropathy and developed severe constipation, urinary retention, and confusion. Her doctor didn’t realize it was the medication. After switching to duloxetine, her symptoms vanished in two weeks. No surgery. No scans. Just a smarter prescription.
Why Doctors Miss These Risks
It’s not negligence. It’s complexity. A senior might see four different specialists: a cardiologist, a neurologist, a rheumatologist, and a primary care doctor. Each prescribes what they think is best for their specialty. No one looks at the full list.
Medicare beneficiaries take an average of five medications daily. One in four take ten or more. That’s polypharmacy-and it’s a recipe for disaster. Drug interactions multiply. Side effects overlap. A blood pressure pill might make you dizzy. A painkiller might make you constipated. A sleep aid might make you forget where you are.
Worse, 58% of seniors don’t know they’re on a high-risk medication. Only 32% say their doctor ever explained the risks. Many assume if it’s on the label, it’s safe.
What You Can Do: The Brown Bag Review
Here’s how to take control: Do a brown bag review every three months.
- Ask your loved one to gather all medications-prescription, over-the-counter, vitamins, supplements, herbal remedies-in a brown paper bag.
- Go to the primary care doctor or a pharmacist (preferably one who specializes in geriatrics).
- Ask: ‘Is any of this on the Beers Criteria list? Is there a safer alternative?’
- Ask about anticholinergic burden. Request a score using the Anticholinergic Risk Scale.
- Ask: ‘Which of these can I stop or replace?’
Pharmacist-led reviews reduce high-risk medication use by 35% within six months. That’s not small. That’s life-changing.
Safer Alternatives That Actually Work
You don’t have to live with poor sleep, pain, or incontinence. Safer options exist.
- For sleep: Skip zolpidem. Try trazodone (low dose), melatonin (3 mg), or CBT-I (cognitive behavioral therapy for insomnia). CBT-I is as effective as pills-with no side effects.
- For diabetes: Swap glyburide for glipizide, metformin, or semaglutide. Glipizide has a much lower risk of low blood sugar.
- For allergies: Replace diphenhydramine with loratadine (Claritin®) or cetirizine (Zyrtec®). No drowsiness. No brain fog.
- For nausea: Skip promethazine. Use ondansetron (Zofran®). It’s safer, more effective, and doesn’t cause tremors.
- For overactive bladder: Avoid oxybutynin. Try mirabegron (Myrbetriq®) or behavioral therapy. Fewer dry mouth, constipation, and confusion side effects.
These aren’t theoretical. Real patients report better energy, fewer falls, clearer thinking, and more independence after switching.

What’s Changing in 2025
The rules are tightening. In January 2024, Medicare Advantage plans started tying 5% of their quality bonuses to reducing high-risk medication use. Pharmacies now use real-time alerts through tools like Surescripts. When a doctor tries to prescribe zolpidem to a 72-year-old, the system flags it and suggests alternatives.
Electronic health records from Epic and Cerner now auto-populate Beers Criteria alerts. If a patient is over 65 and has kidney issues, the system won’t let nitrofurantoin be prescribed without a warning.
The FDA added a black box warning to glyburide in June 2023. That’s the strongest possible alert. It means: This drug can kill older adults.
When to Act Immediately
Don’t wait for a yearly checkup. If your loved one has:
- Fallen in the last six months
- Been confused or disoriented after taking a new pill
- Had a hospital visit for low blood sugar or urinary retention
- Been prescribed more than five medications
- Been taking diphenhydramine or zolpidem for more than a month
Then schedule a medication review today. Don’t wait. Every day on a high-risk drug is another day of avoidable danger.
Final Thought: It’s Not About Taking Less-It’s About Taking Better
Medication isn’t the enemy. The enemy is outdated, one-size-fits-all prescribing. Seniors deserve treatments that match their body’s new reality. A pill that helped at 50 might be harming at 80. Reviewing medications isn’t about cutting corners-it’s about protecting dignity, independence, and life.
Ask the questions. Bring the brown bag. Push for alternatives. You might just save someone’s life-or their ability to walk, think, and live without fear.
What is the Beers Criteria?
The Beers Criteria is a list of medications that are potentially inappropriate for adults aged 65 and older, developed and updated every two years by the American Geriatrics Society. It identifies drugs with higher risks of side effects like falls, confusion, kidney damage, and low blood sugar in seniors. It’s used by doctors, pharmacists, and Medicare plans to guide safer prescribing.
Can I just stop a high-risk medication on my own?
No. Stopping some medications suddenly can be dangerous. Benzodiazepines, for example, can cause seizures if stopped abruptly. Antidepressants can cause withdrawal symptoms. Always talk to your doctor or pharmacist first. They can help you taper safely, usually over 4 to 6 weeks, and replace it with a safer option.
Are over-the-counter drugs safe for seniors?
Not always. Many OTC products contain diphenhydramine (Benadryl®), which is on the Beers Criteria list. Cold medicines, sleep aids, and allergy pills often have it. Even topical creams like lidocaine patches can be risky if used too often. Always check the active ingredients. If you see diphenhydramine, doxylamine, or chlorpheniramine, look for alternatives.
How do I know if a medication has anticholinergic effects?
Look for the Anticholinergic Cognitive Burden (ACB) scale or Anticholinergic Risk Scale (ARS). Medications with a score of 2 or 3 are high risk. Common ones include amitriptyline, oxybutynin, promethazine, and diphenhydramine. Your pharmacist can check the score for any medication you’re taking. A total score over 3 across all meds means high risk.
Is there a tool to check my medications for free?
Yes. The American Geriatrics Society offers a free Beers Criteria checklist on their website. Many Medicare Part D plans also provide medication reviews through their Medication Therapy Management (MTM) program. You can call your pharmacy or Medicare plan and ask for a free medication review. Pharmacists are trained to spot high-risk drugs and suggest alternatives.
What if my doctor says the medication is necessary?
Ask for specifics: ‘Why this drug over a safer alternative?’ ‘What’s the risk if I stop?’ ‘What happens if I keep taking it?’ If they can’t explain why the benefits outweigh the known risks, get a second opinion. A geriatrician or clinical pharmacist can help you weigh options. You have the right to ask for safer choices.



8 Comments
i had no idea benadryl was on that list. my mom takes it every night for sleep. guess we gotta talk to her dr soon. no more midnight zzz's with a side of dementia 😔
these meds are a scam. big pharma knows seniors are easy targets. they push these pills like candy. our grandparents are getting poisoned by profit-driven nonsense. time to call out the corporations and demand real care.
my aunt was on glyburide for years. one bad low sugar episode and she ended up in the er. we switched her to metformin and she’s been walking better than ever. just ask your dr for alternatives - they don’t always know what’s out there. you’re not being difficult, you’re being smart 💛
sooo many people don’t even know what’s in their medicine cabinet 😳 i literally had to throw out 3 bottles of 'sleep aid' with diphenhydramine last week. my grandma thought it was 'just a little help'... nope. nope. nope. 🚫💊
the brown bag review is the single most effective intervention for polypharmacy in older adults. studies show a 35% reduction in high-risk prescriptions within six months when pharmacists are involved. this is evidence-based, low-cost, and scalable. if you’re caring for an elderly person, do this now.
i’ve seen this happen too many times. a 70-year-old on 12 meds. no one ever sat down and said, 'what’s actually helping?' i took my dad’s list to his pharmacist. we cut 4 meds. he sleeps better, walks steadier, and doesn’t feel like a walking pharmacy.
as someone from india, i find this incredibly relevant. here too, seniors are often prescribed multiple drugs without review. the cultural tendency to trust doctors without question can be dangerous. education and open dialogue are key. thank you for sharing this vital information - it could save lives across borders.
my uncle took nitrofurantoin for a uti and ended up in icu with lung damage. kidney function was low but no one checked. this needs to be common knowledge. if you’re over 65, ask your dr: 'is this on the beers list?' simple. life-saving.