
When your knee suddenly gives out during a soccer game, or you hear a loud pop while landing from a jump, it’s not just a bad bruise. It’s a signal that something serious has happened inside your knee. Two of the most common and debilitating injuries - ACL tears and meniscus tears - often happen together, but they’re not the same. One is about stability, the other is about cushioning. And how you treat them changes everything - not just for the next few weeks, but for the next 20 years.
What’s Actually Broken? ACL vs. Meniscus
The ACL (anterior cruciate ligament) is the main rope holding your shinbone in place under your thighbone. It stops your knee from sliding forward and twisting too far. It’s not meant to stretch. When it snaps - usually during a sudden stop, cut, or landing - you feel it. About 90% of people hear a pop. Swelling hits within hours. Your knee feels loose, like it might buckle when you try to turn. The meniscus is different. It’s two rubbery C-shaped pads - one on the inside (medial), one on the outside (lateral) - that act like shock absorbers between your thigh and shin bones. They don’t tear from a single dramatic move. Often, it’s a twist while squatting, kneeling, or even just standing up wrong. You might not feel much at first. But then your knee starts catching. Locking. Swelling comes slower - sometimes not until the next day. That’s a classic sign of a meniscus tear. Here’s the key difference: an ACL tear makes your knee unstable. You can’t trust it. A meniscus tear makes your knee painful and stiff. It might not feel unstable, but it won’t move right.When Do You Need Surgery?
Not every ACL tear needs surgery. But if you’re under 40, active, and want to play sports, run with your kids, or even just walk without fear of your knee giving way - surgery is almost always recommended. Studies show 95% of active people under 40 who skip ACL reconstruction end up with more damage over time - more meniscus tears, more arthritis. Meniscus tears? That’s where things get messy. Only 30-40% of meniscus tears need surgery. The rest? They can heal with rest, physical therapy, and time. But here’s the catch: if the tear is in the outer edge - the red-red zone - where there’s blood flow, repair is possible. If it’s in the center - the white-white zone - where there’s no blood, the tissue can’t heal. That’s when doctors remove the damaged part (meniscectomy). But removing even a small piece of meniscus increases your risk of arthritis later. For every 10% of meniscus removed, your risk of osteoarthritis goes up by 14%. So the big question isn’t just “Can you fix it?” It’s “Should you fix it?”Surgery Options: What’s Actually Inside Your Knee?
ACL reconstruction uses a graft - a piece of tendon taken from your own body. Most common? Hamstring tendon (2,400N strength) or patellar tendon (2,900N strength). Allografts (donor tissue) are faster to recover from initially, but in people under 25, they fail twice as often. A 2023 MOON study found autografts cut re-tear risk by 15% in young athletes. Meniscus repair uses sutures - tiny stitches - to hold the torn edges together. It’s only possible if the tear is in the red zone. The success rate? 89% if done within 8 weeks. Drop to 3 months? It drops to 40-50%. That’s why waiting is dangerous. Delayed treatment increases your chance of needing a partial removal from 35% to 85%. You won’t get a new meniscus. But you can get one repaired - if you act fast.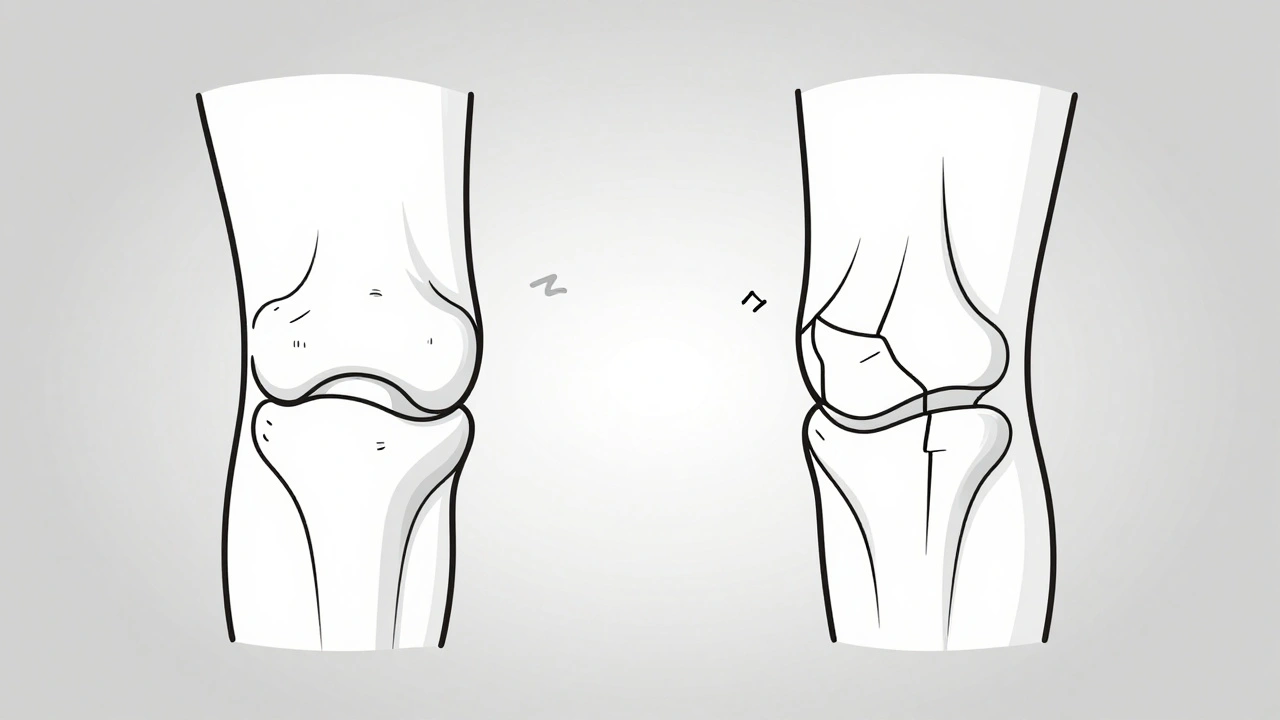
Recovery: The Real Timeline
People think surgery is the finish line. It’s not. It’s the starting line. After ACL reconstruction, you’re not cleared for cutting, jumping, or pivoting until 9 months. That’s not a suggestion. That’s science. A 2023 MOON study found returning before 9 months leads to 18% higher re-injury rates. At 12 months? Re-injury drops to 4.5%. Physical therapy isn’t optional - it’s the difference between getting back to the field and ending up on the sidelines for good. Meniscus repair? Even slower. You can’t put full weight on your leg for 6 weeks. Your knee is locked in a brace, bending only to 90 degrees. That’s brutal. But if you rush it, the repair fails. You end up with a meniscectomy anyway. Meniscectomy? You can walk the next day. Back to work in 2-4 weeks. But you’ll likely have pain when you squat or kneel for years. One Reddit user, u/KneeWarrior99, wrote: “Six months of PT to get 90% strength back. At 12 months, my quad was still 15% smaller than the other leg.” That’s not rare. That’s normal.What Happens If You Don’t Do Anything?
Skipping surgery for an ACL tear doesn’t mean you’ll be fine. It means you’ll be limiting your life. You’ll avoid sports. You’ll stop hiking. You might even stop walking your dog if your knee feels unstable. And over time, the instability wears down your cartilage. By 10 years, 20-30% of people with untreated ACL tears develop osteoarthritis. With meniscus tears, skipping repair doesn’t just mean pain. It means losing your natural shock absorber. Every step you take after a meniscectomy puts more pressure on your joint. That’s why orthopedic groups now say: “Preserve the meniscus whenever possible.” By 2030, experts predict more than half of meniscus tears will be repaired - not removed - because the evidence linking removal to arthritis is too strong to ignore.Cost, Success, and Real Patient Stories
ACL reconstruction costs $15,000-$25,000. Meniscus repair? $9,000-$18,000. Meniscectomy? $6,000-$12,000. Insurance covers most, but deductibles and PT bills add up. Success rates? ACL reconstruction has 82-92% good-to-excellent outcomes at 2 years. But 20-30% develop arthritis within a decade. Meniscectomy has 85-90% short-term satisfaction - but 14% higher arthritis risk per 10% of meniscus removed. One patient, u/MeniscusMom, said: “My meniscus repair took 5 months to get back to soccer. First 6 weeks, I couldn’t bend past 90 degrees. Now I have 20 degrees less extension than my good knee.” She didn’t regret the surgery. But she wished she’d known how long the stiffness would last. Another said: “My surgeon spent an hour explaining graft options. That’s why I trusted him. The PT was brutal, but I didn’t want to be that guy who can’t play with his kids.”What You Can Do Now
If you’ve hurt your knee:- Get an MRI within 2 weeks. Don’t wait. Meniscus repair success drops sharply after 8 weeks.
- Start physical therapy immediately. Even if you’re not sure about surgery, strengthening your quads reduces post-op weakness by 65%.
- Ask your doctor: “Is this tear in the red zone?” If yes, repair is likely possible.
- If you’re over 40 and not active, ask: “Can I manage this without surgery?” Many can.
- Don’t rush back. Nine months isn’t long - it’s the minimum.
What’s Changing in Knee Care
New tools are emerging. Platelet-rich plasma injections are showing 25% higher healing rates in meniscus repairs. Meniscus allografts - transplanting donor meniscus tissue - are helping younger patients avoid arthritis after large removals. And programs like FIFA 11+ are cutting ACL injuries in half among young athletes through neuromuscular training. The future isn’t just about fixing knees. It’s about keeping them intact.Your knee doesn’t need to be perfect. But it needs to be protected. Whether you choose surgery or not, the goal is the same: keep moving - without pain, without fear, without arthritis.


13 Comments
i hurt my knee last year playing basketball and just ignored it for months... dumb move. now i regret it so much. the swelling never went away and i cant even squat without pain. why did i think it would just heal on its own?
The notion that ACL reconstruction is universally necessary for active individuals under 40 is a dangerous oversimplification rooted in outdated orthopedic dogma. The MOON study you cite has significant selection bias, excluding patients who successfully managed non-operative rehab protocols with functional bracing and proprioceptive training. Furthermore, the 95% re-injury statistic conflates return-to-sport failure with structural degradation, ignoring the fact that many athletes adapt their movement patterns and remain asymptomatic without surgical intervention. The medical-industrial complex thrives on surgical intervention, not patient autonomy.
Great breakdown. One thing I wish more people knew: physical therapy isn't just about getting stronger. It's about retraining your brain to trust your knee again. That mental block is real. I did PT for 8 months after my ACL repair. The last 3 months were mostly balance drills and slow single-leg hops. Felt silly. But now I can run without thinking about it. That's the win.
I would like to emphasize, with due respect, that the distinction between the red-red, red-white, and white-white zones of the meniscus is absolutely critical-not merely for surgical decision-making, but for patient expectations. Patients often assume that if a tear is visible on MRI, it is automatically repairable. This is not the case. Blood supply, not tear size or location on imaging, dictates healing potential. Furthermore, the 89% success rate for early repair is contingent upon strict non-weight-bearing protocols; deviating from this reduces success by more than half. Please consult with a specialist who performs >50 meniscus repairs annually.
The biomechanical cascade initiated by meniscectomy is a textbook example of joint homeostasis collapse. The loss of load distribution leads to increased contact pressure, which triggers chondrocyte apoptosis and synovial inflammation-precursors to osteoarthritis. What’s rarely discussed is the neuroplastic component: chronic pain alters motor unit recruitment patterns, leading to quad inhibition and compensatory gait mechanics that accelerate degeneration. We’re not just removing cartilage-we’re rewiring neuromuscular control. That’s why preservation isn’t just orthopedic-it’s neurological.
People who skip surgery are just lazy. They don’t want to put in the work. I had my ACL reconstructed at 22, did 18 months of PT, and now I’m lifting heavier than before. Meanwhile, my cousin ‘waited it out’ and now he can’t even climb stairs without a cane. It’s not hard. It’s just not easy. And if you’re not willing to suffer for your future self, then don’t complain when you’re 40 and stuck on painkillers.
Just got my MRI back-meniscus tear, red zone. Surgeon says I can try PT first. I’m doing it. I’ve seen too many people get removed and regret it. PT is brutal but way better than being the guy who can’t kneel to play with his grandkids. Also-FIFA 11+ is a game changer. My daughter’s team does it before every practice. No ACL injuries this season.
I think it’s important to acknowledge the emotional toll of knee injuries, especially for athletes. It’s not just the physical pain-it’s the loss of identity. I used to run marathons. After my meniscus repair, I could walk again, but the joy was gone for months. I felt broken. It took talking to other athletes in rehab groups to realize I wasn’t alone. Recovery isn’t linear. Some days you feel like a warrior. Others, you just want to cry. Both are valid.
I’m a veteran, had two knee surgeries in my 30s. One thing I’ve learned: your body remembers. Even after everything heals, there’s a part of you that flinches when you twist too fast. That’s okay. It doesn’t mean you failed. It means you survived. I don’t play soccer anymore. But I hike. I garden. I carry my grandkids. And I’m grateful every day for the people who taught me how to move again-not just fix the knee.
This post is a corporate-sponsored PR piece disguised as medical advice. The MOON study? Funded by implant manufacturers. The $25k ACL surgery? That’s the hospital’s markup. Real doctors in Europe do conservative rehab first. You’re being sold a procedure, not a solution. And don’t get me started on PRP injections-placebo with a price tag.
The real tragedy here is not the injury-it’s the societal expectation that we must return to pre-injury performance. We glorify the ‘warrior’ who comes back from ACL tears, but we ignore the quiet ones who choose to live without pain, without pressure, without performance. Why is ‘walking without fear’ not considered a victory? Why must we fix everything? Sometimes, healing is choosing to stop.
My brother had a meniscus repair last year. He followed every PT instruction. No bending past 90 for six weeks. No stairs. No driving. He was miserable. But now, two years later, he’s hiking again. No arthritis. No limp. No regrets. The key? He didn’t rush. He listened. And he didn’t compare his progress to someone else’s. That’s the real secret.
I’m 52, had a meniscectomy 10 years ago. Still play tennis. Still hike. But I don’t squat. I don’t kneel. I don’t run. I’ve learned to live with it. The surgery wasn’t the end. It was the start of a new normal. And honestly? I’m fine with that.