
Every year, over 1.5 million people in the U.S. are harmed by medication errors. Many of these mistakes happen because patients don’t ask the right questions at the pharmacy. It’s not about being suspicious-it’s about being smart. Pharmacists are trained to catch dangerous mistakes before they happen. But they can’t read your mind. If you don’t speak up, they won’t know what you’re worried about.
What is this medication for?
This is the most basic question-and the most overlooked. You might get a prescription for something you’ve never heard of. Maybe your doctor didn’t explain it well, or you were too stressed to remember. Don’t assume. Ask: What is this medication used for? Some drugs have multiple uses. For example, metoprolol is used for high blood pressure, heart rhythm issues, and even migraine prevention. If you’re taking it for one reason but think it’s for another, you might stop it too soon or ignore warning signs. Knowing the purpose helps you track whether it’s working and when to call your doctor.
How and when should I take this?
Dosage instructions aren’t just about how many pills to swallow. They’re about timing, food, and body rhythms. Some meds need to be taken on an empty stomach. Others work best with food. Some must be taken at the same time every day. If you’re told to take a pill "twice daily," does that mean every 12 hours, or just morning and night? Pharmacists can clarify this. One patient took a blood thinner only in the morning, thinking "twice daily" meant morning and evening. Turns out, the correct schedule was every 12 hours. He ended up in the ER with a dangerous bleed. That’s the kind of mistake a simple question could have prevented.
What side effects should I expect?
Not all side effects are bad. Some are normal and fade after a few days. Others are red flags. Ask: What side effects should I expect and which require immediate medical attention? For example, dizziness from a new blood pressure med might be temporary. But if you faint, have chest pain, or your lips turn blue-that’s urgent. Some medications cause skin sensitivity. If you’re on tetracycline or certain diuretics, even a short walk in the sun can give you a bad burn. Your pharmacist will know which ones make you more vulnerable. Don’t wait for Google to tell you what’s dangerous. Ask the expert.
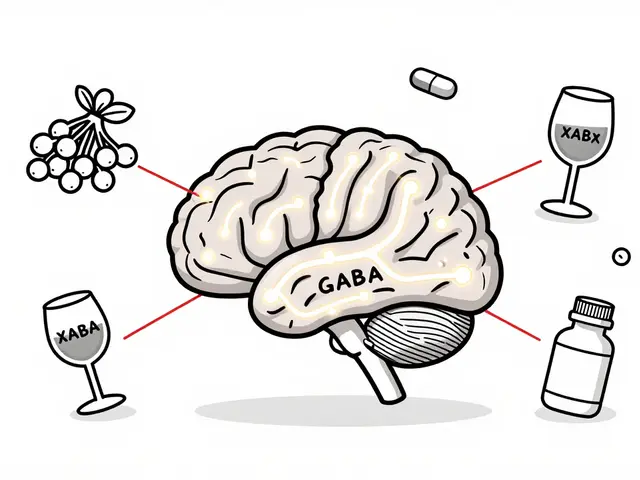
Does this interact with my other meds or supplements?
You might think your vitamins and herbal teas are harmless. They’re not. A 2022 FDA analysis found that combining ibuprofen with blood thinners like warfarin increases the risk of internal bleeding by 40-60%. St. John’s wort can make antidepressants, birth control, and even some heart meds stop working. Even common things like grapefruit juice can interfere with cholesterol and blood pressure drugs. Bring your entire medication list-not just prescriptions. Include over-the-counter painkillers, sleep aids, eye drops, patches, and herbal supplements. Pharmacists check for interactions you didn’t even know existed. One patient in Pennsylvania discovered his fish oil supplement was making his blood thinner too strong. He was lucky he asked before he had a stroke.
Is there anything in this pill that could cause an allergic reaction?
Allergies aren’t just about peanuts or shellfish. Medications contain fillers, dyes, and inactive ingredients that can trigger reactions. Red dye #40, lactose, and gluten are common culprits. If you’ve ever broken out in hives after taking a pill, or had swelling in your throat, you might not realize it was the dye-not the active drug. The CDC says medication allergies lead to over 106,000 emergency room visits each year. Ask: Is there any ingredient that might cause allergic reactions? Pharmacists can tell you if your pill contains gluten, dyes, or other allergens. If you’re unsure, ask for a different brand or formulation. It’s your right.

How should I store this medication?
Leaving pills in the bathroom cabinet? Storing insulin in your car glovebox? That’s not safe. Heat, moisture, and light can ruin medicine. Insulin, for example, becomes useless if it gets too warm. Antibiotics like amoxicillin can lose potency if not refrigerated. Some pills break down in humidity. Your pharmacist can tell you exactly where to keep each one. A pharmacist in Wisconsin recalled a patient who kept his thyroid medication in his glovebox all winter. The cold made it ineffective. He kept feeling tired, didn’t know why-until the pharmacist asked about storage. That’s the kind of fix that takes five seconds to ask and a lifetime to prevent.
Can I repeat back what you just told me?
This one might feel awkward. But it works. A 2020 study in the Journal of the American Pharmacists Association found that when patients repeated instructions back to pharmacists, communication errors dropped by 31%. Say: May I repeat back what you just told me to make sure I understand? It’s not about doubting them-it’s about confirming. If you say, "So I take this once a day with food, and if I get dizzy, I should call you?" and they correct you, you just avoided a mistake. Pharmacists say this simple habit is one of the most effective safety tools they’ve seen. Don’t be shy. They’ve heard it a thousand times-and they’ll appreciate you for it.
Does this look right?
Pharmacies make mistakes. Pills get mixed up. Labels get printed wrong. That’s why you should always check what you’re handed. Ask: Does this look right? Compare the shape, color, and imprint to your last bottle. If it’s different, ask why. The Institute for Safe Medication Practices says 18% of dispensing errors happen because the pill looks wrong-but patients don’t notice. One woman in Ohio picked up her blood pressure med and thought, "This pill is orange now? Last time it was white." She asked. Turns out, the pharmacy had accidentally filled her prescription with a different drug. She was lucky. Another patient took the wrong pill for three weeks and ended up in the hospital.
What if I miss a dose?
Life happens. You forget. You’re traveling. You’re sick. You don’t know what to do. Don’t guess. Ask: What should I do if I miss a dose? Some meds you can take right away. Others you should skip entirely. Doubling up on painkillers or blood thinners can be deadly. Your pharmacist will tell you the safe way to handle it. If you’re unsure, call before you take another pill. Better safe than sorry.

Is there a cheaper or safer alternative?
Cost shouldn’t make you skip doses. Ask: Is there a cheaper or safer alternative? Many drugs have generic versions that work just as well. Some have lower-dose options or different formulations-like patches or liquids-that are easier to take. Pharmacists know about patient assistance programs, coupons, and mail-order options. One man in Florida was paying $120 a month for his diabetes med. His pharmacist found a generic that cost $12. He started taking it regularly. His blood sugar stabilized. He saved over $1,000 a year. That’s the kind of help pharmacists offer-if you ask.
What should I do if I feel worse after starting this?
Some people assume side effects mean the drug is "working." That’s not true. If you feel worse-more tired, more anxious, nauseous, or confused-don’t wait. Ask: What should I do if I feel worse after starting this? Some medications cause depression, confusion, or muscle weakness. These aren’t normal. They’re signs something’s wrong. One woman started a new cholesterol drug and began having memory lapses. She thought it was aging. Her pharmacist asked about her symptoms and realized the drug was linked to cognitive side effects. She switched meds. Her memory came back. Don’t ignore how you feel. Your pharmacist is your best ally.
Bring your whole medicine cabinet
Don’t just bring your new prescription. Bring everything. All your pills, vitamins, creams, eye drops, patches, and herbal teas. A 2022 Johns Hopkins study found that when patients brought all their meds to appointments, polypharmacy risks dropped by 29%. Pharmacists can spot overlaps, duplications, and dangerous combos you didn’t know about. One patient thought he was only taking four meds. He actually had eight-some he forgot about, some his wife gave him, some he bought online. The pharmacist found three dangerous interactions. That’s why you need to show up with your whole cabinet. It’s not weird. It’s smart.
Keep a written list
Write down every medication you take: name, dose, how often, why you take it. Update it every time something changes. Keep it in your wallet or phone. Use it at every doctor’s visit and every pharmacy trip. The University of Rochester found that 56% of hospital admissions involve medication errors-most because the patient couldn’t remember what they were taking. A written list cuts that risk in half. You don’t need an app. Just a piece of paper. But use it.
Ask questions. Always.
You are the most important part of your own safety. Pharmacists are experts-but they can’t fix what they don’t know. If you’re unsure, ask. If you’re nervous, ask anyway. If you’re rushed, ask anyway. You’re not bothering them. You’re helping them help you. The more you ask, the safer you are. And in a world where medication errors are one of the leading causes of preventable harm, that’s not just smart. It’s essential.



9 Comments
You people are so naive. You think asking questions is enough? Half the pharmacists I’ve dealt with don’t even know what half these drugs do-they’re just scanning barcodes and reading off scripts. I’ve seen them hand out antibiotics for viral infections and not even blink. Asking questions doesn’t fix a broken system-it just makes you feel better while they’re still getting paid to mess you up.
And don’t get me started on the ‘repeat back’ nonsense. I once repeated a dosage instruction to a pharmacist who said, ‘Oh, you’re right, I misread that.’ Then she handed me the wrong bottle anyway. She didn’t care. She was on break. You think your ‘smart’ questions matter when they’re clocking out in 12 minutes?
Real safety? It’s not asking. It’s demanding. It’s calling the state board when they mess up. It’s refusing to leave until they call the doctor. It’s bringing a lawyer with you if you’re on five meds. You’re not ‘being smart.’ You’re being polite to people who don’t give a damn.
And yes, I’ve been hospitalized twice because of pharmacy errors. So don’t give me that ‘just ask’ pep talk. I’ve been there. It doesn’t work. The system’s rigged.
Stop trusting the counter. Start documenting everything. Film it. Record the label. Take pictures. And if they give you side-eye? File a complaint. That’s the only way this stops.
I really appreciate how thorough this post is. I used to be the person who just grabbed the bottle and left-until my mom had a bad reaction to a new blood pressure med because she didn’t know it interacted with her thyroid pill. She didn’t even realize she was taking both.
Since then, I bring a little notebook to every pharmacy visit. I write down the name, dose, reason, and any side effects they mention. Sometimes I even draw little icons next to them-like a sun for ‘take with food’ or a moon for ‘take at bedtime.’ It sounds silly, but it helps.
Also, I always ask if there’s a generic. My insurance changes every year, and I’ve saved hundreds just by asking. Pharmacists are way more helpful than people think-they just need you to show up prepared.
Thanks for reminding us that it’s okay to ask. Even if it feels awkward, it’s worth it.
Ive been to 3 different pharmacies in the last 6 months and each one gave me a different pill for the same prescription. One time i got a blue oval one. Next time it was a white round one. Next time it was green. I asked and they said oh its the same thing. NO IT WASNT. The white one had a different active ingredient. I almost died. I dont trust these places anymore. I just get my meds from the VA now. They actually know what theyre doing. The private ones are just profit machines. Also why do they put gluten in everything. Im not celiac but i get bloated. They dont care. Just give me the cheapest crap. I hate this system.
OMG YES. I took my grandma’s meds to the pharmacy once because she was confused and forgot what she was on. The pharmacist looked at the pile-17 bottles-and just said, ‘Wow. You’re on a lot.’ No follow-up. No questions. No ‘let me check for interactions.’
So I did it myself. I made a spreadsheet. Colors, shapes, times, reasons. I printed it. I handed it to them. They were stunned. Then they said, ‘We’ve never had someone do this.’
Turns out two of her meds were duplicates. One was expired. One was for a dog. She’d been taking her dog’s heart pill for three months. I almost cried.
Don’t be shy. Bring the whole cabinet. Even the weird stuff. Even the stuff you think is ‘just herbal.’ They’ll thank you. Seriously.
This is such an important reminder. I work in healthcare admin, and I’ve seen how often medication errors happen-not because pharmacists are careless, but because patients don’t speak up. And honestly, it’s intimidating. You’re sick, you’re tired, you’re overwhelmed, and now you’re supposed to interrogate someone who’s supposed to be helping you?
But the truth is, the more you ask, the more they respect you. I’ve seen pharmacists go out of their way to call doctors, find coupons, or even hand-write instructions for elderly patients who can’t read small print.
One thing I wish more people did: bring a friend or family member. Just one person to listen, take notes, and ask the questions you’re too stressed to think of. It makes a world of difference.
And yes, asking ‘Does this look right?’ saved my sister’s life. The pill looked different. She asked. Turned out it was a different drug entirely. She didn’t take it. She called. She was fine.
Small questions. Big saves.
I’ve been a pharmacist for 18 years. I’ve seen everything.
People who don’t ask? They’re the ones who end up back in the ER. People who ask? They’re the ones who become the most informed patients-and the ones we love to help.
Most of us didn’t go to school for six years just to hand out pills. We want to make sure you’re safe. But we can’t read your mind. We can’t know you’re allergic to red dye #40 unless you tell us.
And yes, bringing your whole medicine cabinet? That’s not weird. That’s professional. I’ve had patients bring 20 bottles. We spent 45 minutes going through them. One guy found he was taking three different blood thinners. He didn’t know.
Don’t be afraid. We’re on your side. We just need you to show up.
As someone from India where pharmacies often operate without a pharmacist present, this post is eye-opening. In many small towns, medicine is sold by clerks with no medical training. People buy antibiotics like candy. No questions asked.
But I’ve learned that even in places with trained pharmacists, the culture of silence is universal. People fear looking foolish. They think asking questions makes them seem weak.
It’s the opposite. Asking shows strength. It shows you value your life.
I now teach my students: if you don’t understand your medicine, don’t take it. Walk out. Go to another pharmacy. Call your doctor. Repeat back. Write it down.
Medication safety isn’t a privilege. It’s a right. And it starts with one simple question: ‘Why am I taking this?’
The point about checking the pill’s appearance is critical. I once took a generic version of a medication that looked completely different from the brand-name version I’d been on for years. I didn’t question it because I assumed generics were identical. They’re not. The inactive ingredients vary. Some people have reactions to those.
I also learned that ‘twice daily’ doesn’t always mean morning and night. One of my colleagues took a medication labeled ‘twice daily’ at 8 a.m. and 8 p.m., but the correct interval was every 12 hours, meaning 8 a.m. and 8 p.m. only works if you’re on a perfect schedule. If you sleep in or work nights, it’s wrong.
Pharmacists can clarify this. But you have to ask. Not just once. Every time. Even if it’s the same drug. Because the manufacturer changes. The batch changes. The label changes.
Never assume. Always verify.
You know what’s really dangerous? The fact that this entire post treats pharmacists like saints. They’re not. They’re employees. They’re overworked. They’re underpaid. They’re incentivized to push generics, not safety. You think they care if you get hives from red dye #40? They care if they hit their daily quota of prescriptions filled.
And let’s be real-asking questions is performative. It makes YOU feel like you’re in control. But the system? It’s still rigged. The real solution? Universal healthcare. Drug price caps. Mandatory pharmacist-to-patient ratios. Not ‘repeat back’ nonsense.
This post is a Band-Aid on a hemorrhage. It’s not empowering. It’s distracting. Stop putting the burden on patients. Fix the system.
Also, ‘Is there a cheaper alternative?’-that’s not a question. That’s a plea for capitalism to be kinder. It’s not a solution. It’s a symptom.