
Every year, millions of people in New Zealand and around the world reach for an OTC painkiller, antihistamine, or heartburn tablet without thinking twice. But how do you know when it’s safe to self-treat - and when you really need a doctor’s prescription? The line isn’t always clear, and getting it wrong can mean wasted money, delayed relief, or even serious health risks.
What’s the real difference between OTC and prescription meds?
It’s not just about where you buy them. OTC medications are approved by health regulators like the FDA for use without a doctor’s order because they’ve been proven safe for self-care in specific, common situations. Prescription drugs, on the other hand, are stronger, more complex, or carry higher risks - so they need professional oversight.
Take hydrocortisone cream. You can buy 1% strength at any pharmacy for a mild rash. But if your skin condition is severe, your doctor might prescribe 2.5% - and that higher dose can cause side effects if used incorrectly. Same active ingredient. Different strength. Different risk level.
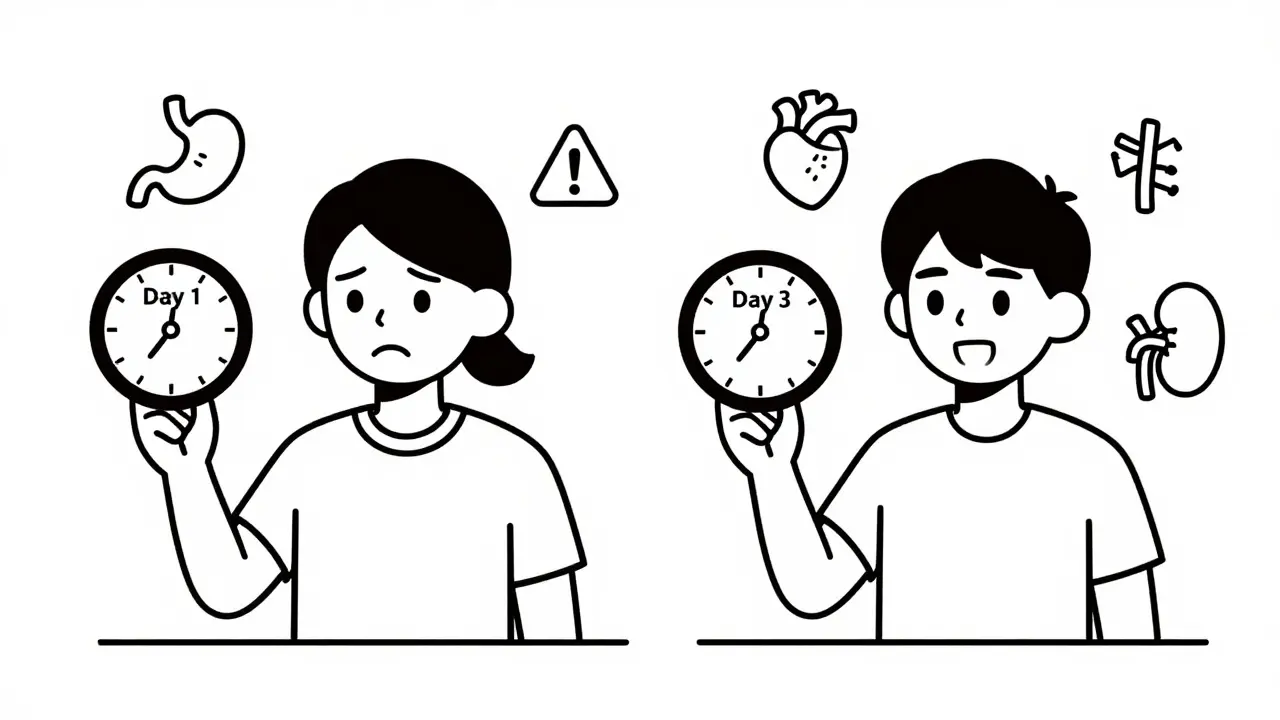
Another example: ibuprofen. OTC versions come in 200 mg tablets. Prescription strength can be 400 mg, 600 mg, or even 800 mg. That’s not just a bigger pill - it’s a different level of treatment. Higher doses mean more effective pain control, but also more strain on your stomach, kidneys, and heart.
OTC drugs follow a set of rules called monographs - basically, approved recipes for ingredients, doses, and uses. If a product sticks to those rules, it can be sold without individual review. Prescription drugs go through a much longer, more expensive approval process called a New Drug Application. That’s why prescription meds often cost more - not because they’re "better," but because they’ve been studied in deeper, more complex ways.
When OTC is the right call
OTC medications work best when your symptoms are mild, short-term, and easy to recognize. Think of them as your first line of defense for everyday issues:
- Headaches: If you get the occasional tension headache after a long day, 200 mg of ibuprofen or 500 mg of acetaminophen (Tylenol) will often clear it up. The American Migraine Foundation says OTC pain relievers are perfect for headaches that happen fewer than 10 times a month.
- Cold and flu symptoms: Runny nose? Sore throat? OTC decongestants, antihistamines like loratadine (Claritin), or throat lozenges can ease discomfort while your body fights off the virus.
- Mild allergies: Cetirizine (Zyrtec) or fexofenadine (Allegra) work well for seasonal sneezing and itchy eyes. These started as prescription drugs but switched to OTC after years of safety data showed they were safe for public use.
- Heartburn: OTC antacids like calcium carbonate (Tums) or H2 blockers like famotidine (Pepcid) are fine for occasional acid reflux. Even the OTC version of esomeprazole (Nexium) works - but only if you give it time. It can take 1-2 days to build up full effect.
- Mild joint or muscle pain: Topical creams with menthol or capsaicin, or oral NSAIDs like naproxen (Aleve), help with stiffness from overuse or minor injury.
Here’s the key: if your symptoms started slowly, aren’t getting worse, and don’t interfere with daily life - OTC is usually fine. And if you’re paying out of pocket, OTC generics often cost less than brand-name versions. A 100-tablet bottle of generic ibuprofen 200 mg can be as cheap as $4. Compare that to a brand-name box of Advil - same dose, same effect, but often triple the price.
When you need a prescription
Don’t wait too long. If OTC meds aren’t helping after 7-10 days, or if your symptoms are getting worse, it’s time to see a professional. Prescription medications are designed for situations where:
- Symptoms are severe or persistent: Chronic migraines, frequent heartburn, or arthritis pain that limits movement need stronger, targeted treatment. For migraines, OTC painkillers might take 30-60 minutes to work. Prescription triptans can work in 20 minutes and stop the attack from progressing.
- Underlying conditions exist: If you have high blood pressure, diabetes, kidney disease, or are on other meds, mixing OTC drugs can be dangerous. Your doctor knows your full history and can pick the safest option.
- Diagnosis isn’t obvious: A rash that won’t go away? Persistent cough? Unexplained fatigue? These aren’t things to guess at. A prescription often comes with a diagnosis - and sometimes, tests to confirm it.
- Control matters: Medications for asthma, thyroid issues, depression, or high cholesterol need regular monitoring. You can’t safely manage these on your own.
There’s also the issue of dosage and delivery. OTC migraine meds are usually pills. Prescription triptans can come as nasal sprays or injections - faster, more reliable for sudden, intense attacks. Same condition. Different tools.
The Rx-to-OTC switch: What’s changing
Over the last decade, more prescription drugs have become available without a prescription. Why? Because safety data proved they could be used safely by the public.
Examples:
- Fexofenadine (Allegra) - switched in 2011
- Esomeprazole (Nexium) - switched in 2014
- Adapalene (Differin) - switched in 2016 for acne
- Epinephrine auto-injectors (EpiPen) - approved for OTC sale in April 2023
This trend is accelerating. Experts predict 20-25 more medications will switch from prescription to OTC by 2030 - especially for allergies, heartburn, and skin conditions. It’s a sign that public health systems are recognizing that people want more control over minor health issues.
But here’s the catch: just because a drug is now OTC doesn’t mean it’s right for everyone. The OTC version of esomeprazole is the same active ingredient as the prescription one - but it’s usually lower dose and meant for short-term use. If you’ve been taking prescription Nexium for years and switch to OTC without talking to your doctor, you might not get the same relief - or you might mask something more serious.
Cost myths and hidden truths
Many people assume OTC is always cheaper. Not always.
Yes, generic ibuprofen costs pennies per pill. But if you’re on Medicare Part D or private insurance, your prescription version might be covered with a $5 copay - making it cheaper than buying OTC every month.
Also, some people buy OTC versions of meds they used to take by prescription - thinking it’s the same. But they don’t realize the dose is lower, or the formulation is slower-release. One Reddit user shared how they switched from prescription omeprazole to OTC and were frustrated when their heartburn didn’t improve in 24 hours. They didn’t know OTC versions take up to 48 hours to build up. Result? They gave up too soon and suffered longer.
Pharmacists are your best resource here. In New Zealand and the U.S., 89% of community pharmacists say they routinely help customers decide between OTC and prescription options. Ask them: "Is this the right strength for me?" or "Could this interact with my other meds?"
What you should never do
Even though OTC meds are easy to get, they’re not harmless. Here are the biggest mistakes people make:
- Assuming "natural" means safe: Herbal supplements and vitamins aren’t regulated like OTC drugs. Some can interfere with prescription meds - like St. John’s Wort with antidepressants.
- Doubling up: Many cold and flu products contain acetaminophen. Taking two different ones can lead to accidental overdose - which can cause liver damage.
- Using OTC for chronic pain: Taking ibuprofen every day for a year? That increases your risk of stomach ulcers and kidney problems. See a doctor.
- Ignoring warning labels: OTC labels now have bigger fonts and clearer warnings (since January 2024). Read them. If it says "don’t use if you have high blood pressure," take it seriously.
How to make the right choice
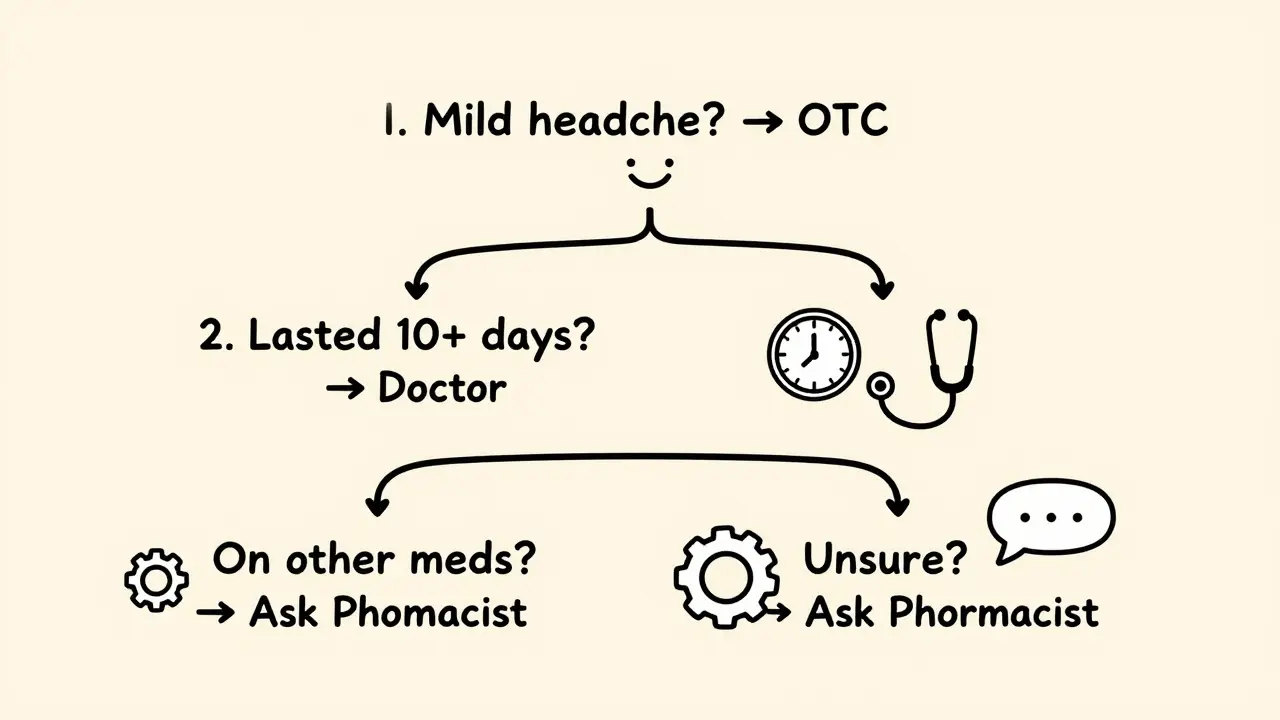
Here’s a simple decision tree:
- Is this a new, mild symptom? (e.g., headache after stress, occasional heartburn, seasonal sneezing) → Try OTC.
- Did it start suddenly and feel severe? (e.g., chest pain, sudden weakness, trouble breathing) → Go to a doctor or ER. Not an OTC situation.
- Has it lasted more than 7-10 days? → See a professional. OTC isn’t working - something else might be going on.
- Are you on other medications or have a chronic condition? → Always check with your doctor or pharmacist before starting any new OTC drug.
- Are you unsure? → Ask your pharmacist. They’re trained to help with this exact question.
The goal isn’t to avoid doctors. It’s to use the right tool for the job. OTC meds are great for quick fixes. Prescription meds are essential for deeper problems. Both have their place - and knowing which is which saves time, money, and health.
Can I just take a higher dose of OTC medicine if it’s not working?
No. Never exceed the maximum daily dose on the label. OTC drugs have safety limits built in. Taking more won’t make them work faster - it just increases your risk of side effects like liver damage (from too much acetaminophen) or stomach bleeding (from too much ibuprofen). If OTC meds aren’t helping, it’s time to see a doctor - not take more pills.
Why do some OTC meds take days to work?
Some OTC drugs, like esomeprazole (Nexium) or certain allergy meds, are designed to build up in your system over time. They’re not meant for instant relief. For example, esomeprazole reduces stomach acid production gradually - so you might not feel better until day two or three. If you expect immediate results like an antacid, you’ll be disappointed. Always read the label for how long it takes to work.
Is it safe to use OTC painkillers every day?
No. Daily use of NSAIDs like ibuprofen or naproxen increases your risk of stomach ulcers, kidney damage, and high blood pressure. If you need pain relief every day, you’re treating a symptom - not the cause. That’s a sign you need to see a doctor to find out what’s really going on. Chronic pain isn’t something to manage with OTC pills long-term.
Can I switch from a prescription to OTC version of the same drug?
Sometimes, but not always. For example, you can switch from prescription fexofenadine to OTC Allegra - same drug, same dose. But if your prescription was a higher strength or extended-release version, the OTC version might not be enough. Always check with your doctor or pharmacist before switching. The OTC version may be meant for short-term use only.
What should I do if I accidentally take too much OTC medicine?
Call your local poison control center immediately. In New Zealand, that’s 0800 POISON (0800 764 766). Don’t wait for symptoms. Acetaminophen overdose, for example, can damage your liver before you feel anything. Bring the medicine bottle with you if you go to the hospital. Many people don’t realize how easy it is to overdose when combining cold meds, painkillers, and sleep aids.
Are OTC medications safer than prescription ones?
Not necessarily. Both are regulated and safe when used correctly. The difference is in how they’re used. OTC drugs are approved for self-care in low-risk situations. Prescription drugs are for more complex or serious conditions. A prescription isn’t "stronger" by default - it’s just meant for situations where professional oversight is needed. Misusing an OTC drug can be just as dangerous as misusing a prescription one.
Final takeaway
OTC medications are powerful tools - but they’re not magic. They’re designed for simple, short-term problems. If your condition is persistent, worsening, or affecting your daily life, don’t keep reaching for the same bottle. Talk to a doctor. Your body is telling you something. Listen to it - and use the right tool for the job.



