
Every year, thousands of people end up in emergency rooms because of a sudden, severe reaction to something they ate. It’s not food poisoning. It’s not indigestion. It’s an IgE-mediated food allergy - and in the worst cases, it leads to anaphylaxis, a life-threatening emergency that can strike in minutes. If you or someone you care about has a food allergy, understanding how these reactions work and how to stop them before they start isn’t just helpful - it’s essential.
What Exactly Is an IgE Food Allergy?
An IgE food allergy happens when your immune system gets it wrong. Instead of recognizing a harmless food protein - like peanut, egg, or milk - as safe, it treats it like an invader. It produces a specific antibody called immunoglobulin E (IgE) to fight it. The next time you eat that food, the IgE antibodies on your mast cells and basophils see the allergen, bind to it, and trigger a chemical explosion. Histamine, leukotrienes, and other inflammatory signals flood your body within seconds to two hours.
This isn’t a slow burn. It’s a rapid cascade. You might get hives on your skin, swelling around your lips or throat, vomiting, wheezing, or a sudden drop in blood pressure. In severe cases, your airway closes, your heart struggles to pump, and you go into anaphylaxis. Unlike delayed reactions (like eczema flares from dairy), IgE reactions are fast, predictable, and can be deadly if not treated immediately.
What Foods Trigger the Most Reactions?
The big eight allergens - milk, egg, peanut, tree nuts, soy, wheat, fish, and shellfish - cause over 90% of serious reactions. But which ones affect you depends on your age.
In young children, milk and egg are the most common. About 2.5% of kids under three are allergic to milk, and nearly 2% react to egg. Peanut allergies affect around 2.2% of children. Many outgrow milk and egg allergies by age 10 or 12 - especially if they can tolerate baked versions. But peanut and tree nut allergies? Only about 1 in 5 kids outgrow them.
By adulthood, shellfish takes the lead. Nearly 3% of adults are allergic to shrimp, crab, or lobster. Tree nuts remain a major concern, affecting 1.8% of adults. Unlike childhood allergies, adult-onset food allergies are less likely to fade. Once you’re allergic to peanuts or shellfish as an adult, it’s usually for life.
How Do You Know It’s an IgE Reaction?
Diagnosis starts with your story. Did your child break out in hives five minutes after eating peanut butter? Did you feel your throat close after eating shrimp? That’s a red flag. But symptoms alone aren’t enough. Doctors use skin prick tests and blood tests to measure IgE levels.
A skin prick test gives a quick result: a raised bump (wheal) bigger than 3mm compared to a control means possible allergy. But it’s not perfect. A positive test doesn’t always mean you’ll react when you eat the food - it just means your immune system has seen it before.
Blood tests measure specific IgE in kU/L. For peanut, a level of 14 kU/L or higher means a 95% chance you’ll react if you eat it. For egg, it’s 7 kU/L. But the real game-changer is component-resolved diagnostics. Testing for specific proteins - like Ara h 2 in peanuts or Gal d 2 in egg - gives better insight into how severe your allergy might be. High levels of Ara h 2? That’s a strong predictor of anaphylaxis.
The gold standard? An oral food challenge. Done under medical supervision, you eat increasing amounts of the food while being monitored. It’s the only way to be 100% sure. But it’s risky - about 1 in 7 people need epinephrine during the test. That’s why it’s only done when needed.

Can You Prevent Food Allergies Before They Start?
For decades, doctors told parents to delay allergenic foods. That advice is now completely wrong - and the evidence is clear.
The landmark LEAP study in 2015 changed everything. Babies at high risk for peanut allergy (those with severe eczema or egg allergy) who started eating peanut-containing foods between 4 and 11 months had an 81% lower chance of developing peanut allergy by age 5. That’s not a small benefit. That’s a revolution.
Current guidelines are simple:
- High-risk infants (severe eczema or egg allergy): Introduce peanut between 4 and 6 months, after seeing a doctor.
- Moderate-risk infants (mild to moderate eczema): Introduce peanut around 6 months.
- Low-risk infants: Introduce peanut along with other solid foods, no need to delay.
The same applies to egg. The EAT study showed introducing cooked egg at 3 months reduced egg allergy by 44% compared to waiting until 6 months.
But here’s the twist: it’s not just about eating. Skin matters too. If your baby has cracked, dry skin from eczema, allergens can sneak in through the barrier and trigger sensitization. That’s why the BEEP trial found daily use of petroleum jelly from birth cut food allergy risk by half in high-risk babies. Keeping skin healthy is just as important as feeding allergens early.
What About Vitamin D, Probiotics, and Other Myths?
You’ve probably heard about probiotics, prenatal vitamins, or avoiding allergens during pregnancy. Let’s cut through the noise.
Probiotics? The Cochrane Review found no reliable evidence they prevent food allergies. Don’t waste your money.
Vitamin D? The data is promising. Babies with vitamin D levels above 30 ng/mL have more regulatory T cells - the immune cells that teach the body to tolerate food. Mothers with vitamin D levels above 75 nmol/L during pregnancy had 30% lower odds of their child developing food sensitization. But we don’t yet have a definitive RCT proving supplementation prevents allergies. Still, maintaining healthy vitamin D levels (through sun, diet, or supplements) is smart for immune health overall.
And no, avoiding peanuts or eggs during pregnancy or breastfeeding doesn’t help. In fact, it might hurt. The theory is simple: early oral exposure = tolerance. Early skin exposure = allergy.
What If You Already Have a Food Allergy?
Avoidance is still the rule - but it’s not enough. Accidental exposures happen. Studies show 50-80% of kids with peanut allergy have at least one accidental ingestion over five years. And 25-35% of those require epinephrine.
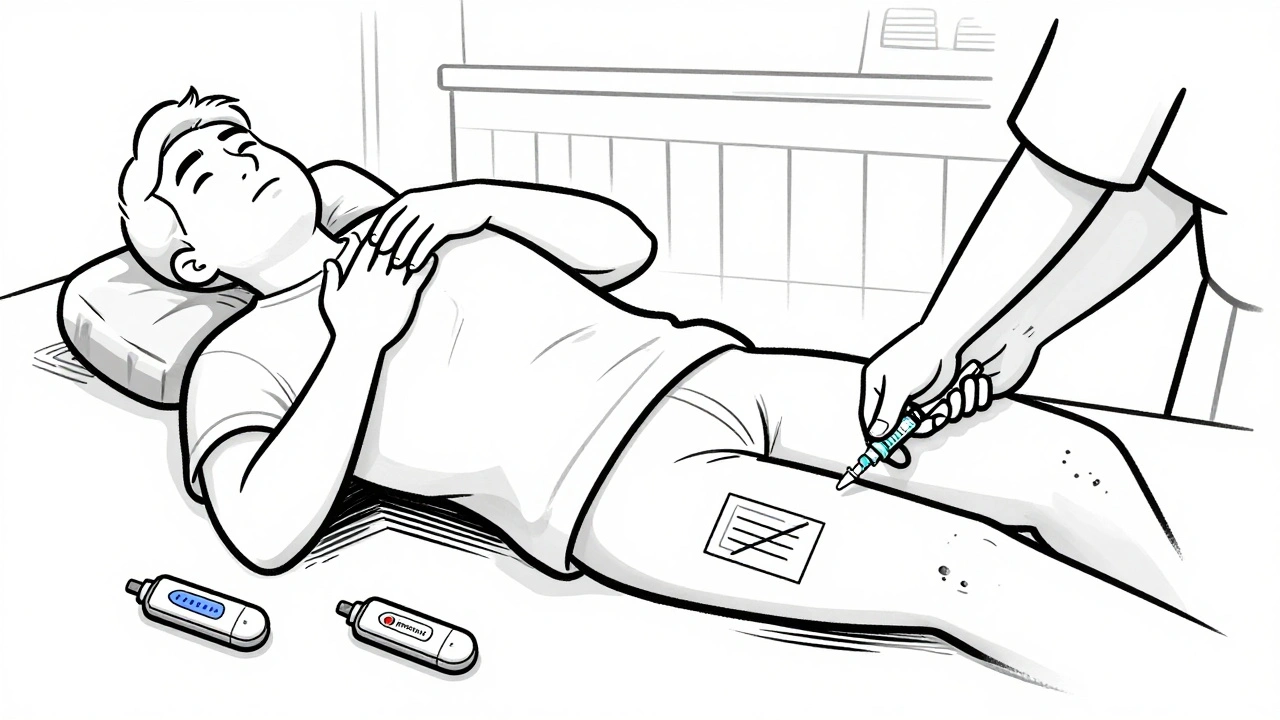
That’s why every person with a known IgE food allergy needs an emergency action plan and two epinephrine auto-injectors - always with them. EpiPen (0.3 mg) for adults and teens over 30 kg. Auvi-Q (0.15 mg) for kids 15-30 kg. Inject into the outer thigh. Don’t wait. Don’t give antihistamines first. Epinephrine is the only thing that stops anaphylaxis.
Delaying epinephrine by more than 30 minutes increases the risk of a second wave of symptoms (biphasic reaction) by 68%. It also triples your chance of needing ICU care.
For long-term management, oral immunotherapy (OIT) is now FDA-approved for peanut allergy in kids 4-17. Palforzia, the peanut powder, helps 67% of users tolerate the equivalent of two peanuts. It’s not a cure - you still need to keep eating it daily. But it reduces the risk of a severe reaction from accidental exposure.
Sublingual immunotherapy (SLIT) and biologics like omalizumab (Xolair) are also options. Omalizumab cuts reaction rates during OIT by half, making the process safer and faster.
How to Prevent Anaphylaxis in Daily Life
Prevention isn’t just about medicine - it’s about habits.
- Always read labels. Ingredients change. “May contain” warnings aren’t legally required, but take them seriously.
- Carry two auto-injectors. One can fail. One can be left at home. Always have a backup.
- Train everyone around you. Teachers, babysitters, family members - they need to know how to use an auto-injector. Don’t assume they will.
- Use wearable tech. New auto-injectors like Auvi-Q give voice instructions during use. In simulations, correct use jumped from 60% to 92%.
- Check school policies. Schools with full food allergy management programs see 32% fewer emergency visits.
And don’t forget: even trace amounts matter. A single peanut can trigger a reaction in the most sensitive. New food-testing tools can now detect allergens as low as 2.5 parts per million - useful for checking restaurant meals or homemade snacks.
What’s Next in Food Allergy Research?
The science is moving fast. The PREPARE trial is testing whether giving pregnant women 4,400 IU of vitamin D daily reduces food allergy in their babies by age 3. The EAT2 study is seeing if introducing six allergens (peanut, egg, milk, sesame, fish, wheat) at 3 months prevents allergies better than single-food introduction.
On the treatment side, researchers are testing TLR9 agonists combined with immunotherapy - early results show 80% desensitization. Nanoparticles that deliver peanut peptides without triggering IgE are also in trials. The goal? Not just desensitization, but true tolerance - where the body forgets the allergen is a threat.
But here’s the sobering truth: even with perfect early introduction, about 20% of children still develop peanut allergies. That means prevention isn’t solved. We need better tools - for skin health, for immune training, for early detection.
Final Thoughts: Knowledge Is Your Shield
Food allergies aren’t going away. But the way we prevent and manage them has changed dramatically in the last decade. Early introduction works. Epinephrine saves lives. Skin care matters. And knowing your triggers - and your emergency plan - can mean the difference between a scare and a tragedy.
If you’re a parent, don’t wait. Talk to your doctor about introducing allergens at the right time. If you or your child already has an allergy, make sure you have two auto-injectors, you know how to use them, and everyone around you does too. This isn’t about fear. It’s about being prepared.
The future of food allergy care is brighter than ever. But right now, your best defense is simple: act early, act smart, and never underestimate the power of epinephrine.




13 Comments
This article is basic. IgE reactions aren't even the whole story. You're ignoring FcεRI signaling pathways and the role of basophil activation in late-phase responses. If you're going to write about anaphylaxis, at least cite the 2022 JACI meta-analysis on mast cell heterogeneity.
I'm so glad this exists. My daughter had her first anaphylaxis at 14 months to peanut butter. We didn't know anything until it was too late. The part about skin health and petroleum jelly? That's what saved us after she developed severe eczema. So grateful for the LEAP study.
I've been doing OIT with my son for 18 months now. Palforzia isn't magic but it's changed our lives. We used to panic every time he licked a spoon that touched peanut butter. Now he can eat a cookie at school without me hyperventilating. Still need the epinephrine, but the fear? It's less now.
In the UK we're still playing catch-up. GP's here don't even mention early introduction unless you bring it up. My niece was only tested at age 4 after three reactions. Shame. We need better public health messaging. The science is clear.
I'm not saying this is wrong, but I've read the original LEAP study and the follow-ups. The population was heavily skewed toward high-risk infants with eczema. Applying this to the general population? That's where the real danger lies. We're creating a generation of parents terrified of feeding their kids anything. And now we have parents who think a single drop of peanut oil is a death sentence. It's not. It's anxiety dressed as science.
Wait so you're telling me I can't even lick my fingers after touching a peanut butter jar? What if I'm a kid with no eczema? Do I need a blood test before eating a cookie? This is insane. I've eaten peanuts my whole life and never had a reaction. Now I'm supposed to be scared of crumbs? You're making people paranoid. It's not a plague. It's a statistical outlier.
I'm a pediatric nurse, and I see this every day. Parents are terrified. They don't know what to do. This article? It's the first one that actually gives them clear steps. The part about carrying two injectors? That's non-negotiable. I had a mom come in last week because she only had one. She didn't know the other one could fail. We need more of this. Not less.
I've been living with this for 27 years. Shellfish. Every summer I get a reaction. Every year I think it's the last. Last year I went into anaphylaxis on a cruise. They gave me epinephrine, but the EpiPen was expired. I had to wait 17 minutes for the ship's doctor. That's not a scare tactic. That's a death sentence waiting to happen. I carry two. Always. I don't care what anyone says. If you have this, you don't get to be casual. You don't get to be 'it's probably fine'. It's not fine. It's never fine.
I appreciate the breakdown. My sister just got diagnosed with tree nut allergy at 32. We thought she was just sensitive to nuts. Turns out it was IgE all along. The component-resolved diagnostics part? That was eye-opening. She tested high for Ara h 2. Now we know why her reactions were so bad. We're getting her on OIT next month. Thanks for the clarity.
The body knows. The mind forgets. Allergies are not mistakes. They are signals. We have forgotten how to listen to the silence between breaths.
So you're saying the entire medical establishment got it wrong for 30 years? That's convenient. What if the real problem is the overuse of antibiotics, glyphosate in food, and the destruction of the microbiome? You're blaming the food, not the system. And now we're feeding babies peanut butter like it's a vaccine? Sounds like corporate pharma pushing another product. Palforzia costs $10,000 a year. Who's really benefiting here?
It is imperative that all caregivers of individuals with IgE-mediated food allergies adhere strictly to the recommended protocols regarding epinephrine administration and allergen avoidance. The data is unequivocal. Delay in epinephrine administration correlates directly with increased morbidity and mortality. This is not a suggestion. It is a medical imperative.
You're telling parents to feed their babies peanuts at 4 months? That's insane. What about the kids who get anaphylaxis on the first bite? You're playing God with children's lives. And now you want to inject them with peanut powder? This isn't medicine. It's a dangerous experiment. I have a 2-year-old. I wouldn't risk it. Not for any study. Not for any doctor. Not for any 'science'.