
Medication Itch Risk Checker
Check Your Medication Risk
This tool helps you identify if your medications might be causing itching based on the article's research on drug-induced pruritus.
Next steps:
For each potential cause, consider the following:
Important: Never stop medication without consulting your doctor. Discuss your symptoms with your provider to explore safe alternatives.
Itching isn’t just a nuisance-it can be relentless, sleep-stealing, and even disabling. When it shows up after starting a new medication, it’s not just bad luck. It’s a known side effect, and one that’s more common than most people realize. You might be taking a pill for high blood pressure, cholesterol, or even an allergy, and suddenly your skin starts screaming. No rash. No bumps. Just pure, unrelenting itch. That’s drug-induced pruritus, and it’s happening to more people than doctors admit.
What’s Really Causing the Itch?
Itching from meds isn’t one thing. It’s a whole list of possibilities. Some drugs trigger it by releasing histamine, the same chemical that makes you sneeze during hay fever. Others mess with your nerves, your liver, or your skin’s natural barrier. The worst part? You won’t always see a rash. That’s why so many people think it’s dry skin, stress, or an allergy to laundry detergent.Here are the big culprits:
- Antibiotics like penicillin and tetracycline
- High blood pressure meds-especially ACE inhibitors and ARBs (like lisinopril or losartan)
- Statins (atorvastatin, simvastatin) for cholesterol
- NSAIDs like aspirin and ibuprofen
- Opioids (morphine, codeine)-especially after surgery or spinal injections
- Antidepressants like amitriptyline and SSRIs
- Antimalarials like chloroquine
- Antihistamines like cetirizine and levocetirizine
Yes, you read that right. Even the pills you take to stop itching can cause it-after you stop taking them. A 2023 FDA warning confirmed that people who’ve been on cetirizine or levocetirizine for months or years can develop severe itching within days of quitting. In 90% of cases, the itch went away when they restarted the drug. That’s not a coincidence. It’s a physiological reaction.
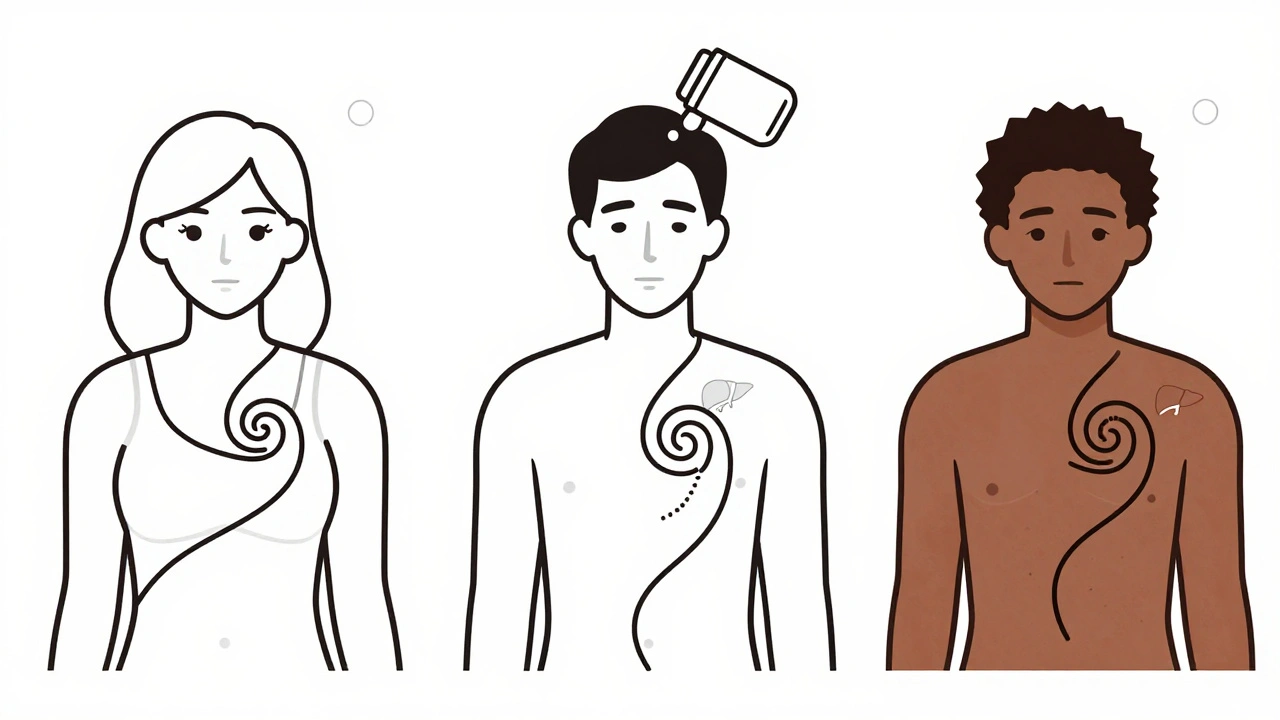
Who’s Most at Risk?
It’s not random. Certain groups are far more likely to experience this. Studies show women are about 70% more likely than men to develop drug-induced itching. Black patients are nearly twice as likely to react compared to white patients-especially with drugs like chloroquine, where up to 90% of Black patients report intense itching during malaria treatment.Age matters too. The longer you’ve been on a medication, the higher your risk. The FDA found that 92% of people who had severe itching from antihistamine withdrawal had been taking the drug for more than three months. Some had been on it for over 20 years. It’s not about dosage-it’s about time. Your body adapts. Then, when you stop, it overreacts.
And it’s not just the drug. Your skin’s condition plays a role. If you already have dry skin, eczema, or psoriasis, medications are more likely to trigger or worsen itching. Moisturizing isn’t just helpful-it’s part of the treatment plan.
How Doctors Diagnose It
There’s no blood test for drug-induced pruritus. No scan. No lab marker. Diagnosis is all about timing and elimination. Did the itching start after you began a new pill? Did it get worse when you increased the dose? Did it vanish after you stopped? That’s the story doctors follow.Here’s how it usually works:
- Make a full list of every medication you take-prescription, over-the-counter, vitamins, supplements. Don’t leave anything out.
- Track when the itching started and how it changed with each drug change.
- Rule out other causes: liver disease, kidney problems, thyroid issues, or skin conditions like eczema.
- If possible, stop the most likely suspect under medical supervision. If the itch fades within days, you’ve found your trigger.
Pharmacists are often the first to spot the pattern. They see your full medication history. They know which drugs are linked to itching. If you’re struggling with unexplained itch, ask your pharmacist to review your list. They can flag the usual suspects before your doctor even thinks to look.
What Happens When You Stop the Drug?
Stopping the medication is the gold standard for confirming the cause. But what if you can’t stop it? Maybe it’s your blood pressure pill, your painkiller, or your antidepressant. You can’t just quit.That’s where things get tricky. For some drugs, like statins or ACE inhibitors, the itching may fade over weeks even if you keep taking them. For others-like opioids or antihistamines-it gets worse without the drug.
The FDA’s data on antihistamine withdrawal is eye-opening. Of the 209 severe cases reported, 92% of people had been taking the drug for more than three months. When they stopped, itching hit within two days. Restarting the drug helped 90% of them. But here’s the catch: only 38% of people who tried tapering off after restarting saw lasting relief. That means for many, the only way to avoid the itch is to stay on the drug-or find a different one.
Treatment Options That Actually Work
There’s no one-size-fits-all fix. What works for one person might do nothing for another. But here’s what the evidence shows:- Topical creams: Moisturizers with ceramides or colloidal oatmeal help if your skin is dry. Capsaicin cream (the stuff in chili peppers) can numb nerve endings and reduce itch. Low-dose steroid creams may help if there’s inflammation.
- Oral antihistamines: These help if histamine is the culprit-but they often don’t work for drug-induced itching. That’s because many cases involve non-histamine pathways. Still, second-generation ones like loratadine or fexofenadine are safe to try.
- Antidepressants: Surprisingly, low-dose amitriptyline or doxepin can calm nerve signals that cause itch. They’re not for depression-they’re for nerves.
- Other nerve modulators: Gabapentin and pregabalin, usually used for nerve pain, have shown success in stubborn cases.
- Light therapy: UVB phototherapy can help in chronic cases, especially if other treatments fail.
For opioid-induced itching, doctors sometimes add an antihistamine like hydroxyzine or use a drug called naloxone to block the itch pathway without reducing pain relief. It’s not magic, but it works for many.
What to Do Right Now
If you’re itching and on meds, don’t panic. Don’t stop your pills without talking to your doctor. But do this:- Write down every medication you take, including doses and when you started.
- Track when the itch started, how bad it is (1-10 scale), and what makes it better or worse.
- Check your skin daily for changes-rash, redness, dryness.
- Moisturize twice a day with a fragrance-free cream.
- Take cool showers. Avoid hot water and harsh soaps.
- Ask your pharmacist to review your meds for itching risks.
- Bring your notes to your doctor. Say: “I think this itch might be from my meds. Can we look at this?”
Most importantly-don’t ignore it. Severe itching has been linked to hospitalizations and even suicidal thoughts in rare cases. It’s not just skin deep. It affects your sleep, your mood, your life.
What’s Changing in 2025
The FDA’s 2023 warning on antihistamine withdrawal was a turning point. Now, labels on cetirizine and levocetirizine packages must mention this risk. That’s new. That’s progress.Doctors are starting to ask about medication history before treating chronic itch. Pharmacists are being trained to spot these patterns. Electronic health records are now flagged to alert providers when a patient on long-term statins or antihypertensives reports itching.
But the real change is in awareness. Patients are speaking up. In the FDA’s data, 87% of the 209 cases were reported by patients themselves-including healthcare workers who recognized the pattern in their own bodies. You don’t need to be a doctor to know when something’s wrong. Trust your skin. Speak up.
When to Worry
Not all itching is dangerous. But if you have:- Itching that started within days of a new drug
- Itching that doesn’t improve with moisturizers or OTC antihistamines
- Itching that wakes you up at night
- Itching with fatigue, dark urine, yellow eyes, or nausea (signs of liver trouble)
- Thoughts of self-harm or extreme distress because of the itch
…then you need to see a doctor immediately. This isn’t something to wait out. It’s a signal.
Can I just stop the medication if it’s causing itching?
No-not without talking to your doctor first. Some medications, like blood pressure or antidepressant drugs, can cause serious rebound effects if stopped suddenly. Always work with your provider to safely adjust or switch your treatment.
Why do antihistamines cause itching after stopping them?
Your body adjusts to the constant presence of the drug. Over time, your nerve pathways become more sensitive to itch signals. When you stop, your system overreacts, flooding your skin with itch signals. It’s like a thermostat that’s been set too high for too long-when you turn it off, the room gets way too cold.
Is itching from statins common?
Yes. About 1 in 10 people on statins report itching, especially in the first few months. It’s often mild and goes away on its own. But for some, it’s severe enough to stop taking the drug. If you’re on a statin and itching starts, don’t assume it’s dry skin. Talk to your doctor about switching to a different statin or trying a non-statin cholesterol option.
Can I use over-the-counter hydrocortisone cream for drug-induced itching?
It might help if your skin is inflamed or dry, but it won’t fix the root cause. Hydrocortisone reduces inflammation, not nerve-based itch. For itching caused by opioids, statins, or antihistamine withdrawal, it’s usually not enough. Use it short-term while you work with your doctor to identify the trigger.
Why is itching worse in Black patients with certain drugs?
Research suggests genetic differences in how the body processes certain drugs and how nerve receptors respond to them. For example, chloroquine binds more strongly to skin receptors in people with darker skin tones, triggering stronger itch signals. It’s not an allergy-it’s a biological difference in drug response. This is why doctors need to consider race and ethnicity when choosing medications.
How long does drug-induced itching last after stopping the medication?
It varies. For most people, itching fades within days to weeks. But in some cases-especially with drugs like hydroxyethyl starch or long-term antihistamine use-it can last for months. One study found itching persisted for up to 15 months after stopping a single infusion. Patience and ongoing treatment are key.
If you’ve been living with unexplained itching and you’re on any long-term medication, you’re not alone. And you’re not imagining it. This is real, documented, and treatable. The next step isn’t to suffer through it-it’s to ask the right questions and demand answers.



15 Comments
Itching isn't just a side effect-it's your body screaming that the drug is rewriting your nervous system's code. We treat meds like candy, but they're not. They're chemical intruders. And when your skin starts burning without a rash? That's not dryness. That's your neurons throwing a mutiny.
They say 'trust your skin.' I say trust your nerves. They don't lie. Not like doctors who blame stress or detergent.
I stopped cetirizine after 12 years. Itch hit like a tsunami. No rash. Just raw, sleepless hell. Restarted it? Gone in 48 hours. The FDA finally admitted it. Took 209 cases. Took people nearly losing their minds. Now the label says 'warning.' Should've said 'danger zone.'
Respected sir or madam please accept my humble gratitude for this detailed exposition on drug induced pruritus
It is truly remarkable how modern pharmacology can induce such profound physiological responses without overt dermatological manifestations
One must exercise extreme caution when altering long term medication regimens
Thank you for illuminating this critical yet overlooked aspect of patient care
AMERICA IS THE ONLY COUNTRY WHERE THIS IS EVEN A PROBLEM
EVERY OTHER COUNTRY JUST TELLS YOU TO SUFFER
WE HAVE THE BEST DOCTORS THE BEST PHARMACISTS THE BEST FDA
IF YOU'RE ITCHING YOU'RE JUST WEAK
MY GRANDPA TOOK LISINOPRIL FOR 40 YEARS AND NEVER COMPLAINED
YOU PEOPLE ARE TOO SOFT
STOP WHINING AND TAKE YOUR PILLS
Okay but can we just take a moment to celebrate how amazing it is that we're finally talking about this?
For so long people suffered in silence thinking they were just dry or stressed or crazy
Now we have data we have labels we have doctors listening
And if you're reading this and you've been itching for months? You're not alone
Write down your meds
Ask your pharmacist
Trust your body
You got this
One cannot help but observe the profound cultural and biological disparities in drug-induced pruritus across global populations
It is not merely pharmacological-it is epigenetic
Chloroquine’s interaction with melanin-rich dermal receptors represents a paradigm shift in personalized medicine
Western medicine has long operated under a homogenized model
But now we see: biology does not obey borders
And neither should treatment protocols
This is not bias-it is bio-precision
Let us not mistake difference for deficiency
This article is excessively verbose and lacks academic rigor.
Several claims are cited without peer-reviewed references.
The FDA data mentioned is not publicly accessible in the form described.
Furthermore, the assertion that antihistamine withdrawal causes itching in 90% of cases is statistically implausible without controlled trials.
It is regrettable that such speculative content is presented as authoritative.
"Your body adapts. Then, when you stop, it overreacts."
That’s not a physiological mechanism. That’s a metaphor.
Where’s the receptor downregulation data?
Where’s the histamine receptor binding affinity study?
"Thermostat" analogy? Cute.
But this isn’t a TED Talk. It’s medical literature.
And you’re missing citations.
And you’re misusing "physiological reaction" as a catch-all.
And you didn’t even mention basophil degranulation.
Unprofessional.
MY BEST FRIEND GOT OFF CETIRIZINE AFTER 18 YEARS AND STARTED SCRATCHING HER ARMS OFF AT 3AM
SHE THOUGHT SHE WAS GOING CRAZY
THEN SHE FOUND THIS ARTICLE
SHE WENT BACK ON IT
AND THE ITCHING VANISHED
LIKE MAGIC
DOCTORS AREN’T LISTENING
BUT WE ARE
AND WE’RE NOT ALONE
😭🙏
Write down your meds.
Ask your pharmacist.
Moisturize.
Don’t stop cold.
That’s it.
You don’t need a thesis.
You need action.
This is so important.
I’ve seen people in my community suffer for years thinking it’s just their skin.
No one tells them about meds.
They think it’s shame.
But it’s biology.
Thank you for saying this out loud.
Someone needed to hear it.
Bro I had this exact thing with simvastatin
Itched for 9 months
Thought it was my detergent
Then my cousin who’s a nurse said "have you tried switching statins?"
I switched to pravastatin
POOF
Itch gone
AND I DIDN’T EVEN KNOW STATINS COULD DO THIS
WHY ISN’T THIS ON THE BOX?
AND WHY DO DOCTORS ACT LIKE IT’S IMPOSSIBLE?
MY MOM WAS ON LISINOPRIL FOR 15 YEARS AND SHE ITCHES EVERY SPRING
THEY JUST SAY "USE CREAM"
WE NEED TO CHANGE THIS SYSTEM
im so glad i found this
i been itching for 2 years
thought i was going crazy
took cetirizine for 7 years
stopped for 2 weeks cause i thought i was getting addicted
then i couldnt sleep
skin on fire
started back on it
it was like a miracle
why do they not tell us this?
so many people suffer in silence
I didn’t sleep for 17 nights.
I scratched until I bled.
I cried every night.
I thought I was broken.
I thought I deserved it.
Then I read about antihistamine withdrawal.
I went back on the drug.
It didn’t fix me.
It saved me.
I’m not okay.
But I’m alive.
And I’m not alone.
Just took my mom to the doc yesterday
She’s been itching for 8 months
Doc said "dry skin"
She showed him this article
He paused
Then said "huh. I didn’t know that."
Switched her statin
Itch gone in 5 days
So yeah
It’s real
And we’re the ones who have to teach the doctors
😭✌️
And now the FDA is finally labeling it. But here’s the real tragedy: the people who need this info the most-elderly, low-income, non-English speakers-are the ones who never see it.
It’s not enough to have a warning on the bottle.
You need a pamphlet in the pharmacy. A nurse at the clinic. A text alert when you refill.
Knowledge is power.
But power means nothing if it’s locked behind a prescription bottle and a 10-page consent form.
We need systems.
Not just articles.
Not just hashtags.
Real infrastructure.
Because someone’s skin is still screaming right now.
And they’re still alone.